Endocrine system
Provides chemical communications within the body using
| Endocrine system | |
|---|---|

Main glands of the endocrine system
| |
| Details | |
| Latin | Systema endocrinum |
| Identifiers | |
| FMA | 9668 |
| Anatomical terminology | |
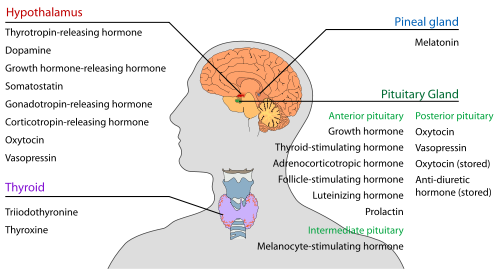
The endocrine system refers to the collection of glands of an organism that secrete hormones directly into the circulatory system to be carried towards distant target organs. The major endocrine glands include the pineal gland,pituitary gland, pancreas, ovaries, testes, thyroid gland, parathyroid gland,hypothalamus, gastrointestinal tract and adrenal glands. The endocrine system is in contrast to the exocrine system, which secretes its hormones using ducts. The endocrine system is an information signal system like the nervous system, yet its effects and mechanism are classifiably different. The endocrine system's effects are slow to initiate, and prolonged in their response, lasting from a few hours up to weeks. The nervous system sends information very quickly, and responses are generally short lived. In vertebrates, the hypothalamus is the neural control center for all endocrine systems. The field of study dealing with the endocrine system and its disorders is endocrinology, a branch of internal medicine.
Special features of endocrine glands are, in general, their ductless nature, their vascularity, and commonly the presence of intracellular vacuoles or granules that store their hormones. In contrast, exocrine glands, such assalivary glands, sweat glands, and glands within the gastrointestinal tract, tend to be much less vascular and have ducts or a hollow lumen.
In addition to the specialised endocrine organs mentioned above, many other organs that are part of other body systems, such as bone, kidney, liver, heartand gonads, have secondary endocrine functions. For example the kidney secretes endocrine hormones such as erythropoietin and renin.
A number of glands that signal each other in sequence are usually referred to as an axis, for example, the hypothalamic-pituitary-adrenal axis.
As opposed to endocrine factors that travel considerably longer distances via the circulatory system, other signaling molecules, such as paracrine factors involved in paracrine signalling diffuse over a relatively short distance.
The word endocrine derives from the Greek words ἐνδο- endo- "inside, within," and κρίνειν krinein "to separate, distinguish".
Contents
[hide]- 1 Endocrine organs and known secreted hormones
- 2 Targets
- 3 Diffuse neuro-endocrine system (DNES)
- 4 Major endocrine systems
- 5 Interaction with immune system
- 6 In other species
- 7 Diseases
- 8 Other types of signaling
- 9 Additional images
- 10 See also
- 11 References
- 12 External links
Endocrine organs and known secreted hormones
Hypothalamus
Pineal body (epiphysis)
| Secreted hormone | From cells | Effect |
|---|---|---|
| Melatonin | Pinealocytes | Antioxidant Monitors the circadian rhythm including induction ofdrowsiness and lowering of the core body temperature |
Pituitary gland (hypophysis)
The pituitary gland (or hypophysis) is an endocrine gland about the size of a pea and weighing 0.5 grams (0.018 oz) in humans. It is a protrusion off the bottom of the hypothalamus at the base of the brain, and rests in a small, bony cavity (sella turcica) covered by a dural fold (diaphragma sellae). The pituitary is functionally connected to the hypothalamus by themedian eminence via a small tube called the infundibular stem or pituitary stalk. The pituitary fossa, in which the pituitary gland sits, is situated in the sphenoid bone in the middle cranial fossa at the base of the brain. The pituitary gland secretes nine hormones that regulate homeostasis and the secretion of other hormones.[citation needed]
Anterior pituitary lobe (adenohypophysis)
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Growth hormone (somatotropin) | GH | Somatotrophs | Stimulates growth and cell reproduction Stimulates Insulin-like growth factor 1 release fromliver |
| Thyroid-stimulating hormone (thyrotropin) | TSH | Thyrotrophs | Stimulates thyroxine (T4) and triiodothyronine (T3) synthesis and release from thyroid gland Stimulates iodine absorption by thyroid gland |
| Adrenocorticotropic hormone (corticotropin) | ACTH | Corticotrophs | Stimulates corticosteroid (glucocorticoid andmineralcorticoid) and androgen synthesis and release from adrenocortical cells |
| Beta-endorphin | – | Corticotrophs | Inhibits perception of pain |
| Follicle-stimulating hormone | FSH | Gonadotrophs | In females: Stimulates maturation of ovarian follicles inovary In males: Stimulates maturation of seminiferous tubules In males: Stimulates spermatogenesis In males: Stimulates production of androgen-binding protein from Sertoli cells of the testes |
| Luteinizing hormone | LH | Gonadotrophs | In females: Stimulates ovulation In females: Stimulates formation of corpus luteum In males: Stimulates testosterone synthesis fromLeydig cells (interstitial cells) |
| Prolactin | PRL | Lactotrophs | Stimulates milk synthesis and release from mammary glands Mediates sexual gratification |
| Melanocyte-stimulating hormone | MSH | Melanotropes in the Pars intermedia of the Anterior Pituitary | Stimulates melanin synthesis and release from skin/hair melanocytes |
Posterior pituitary lobe (neurohypophysis)
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Oxytocin | Magnocellular neurosecretory cells | In females: uterine contraction during birthing,lactation (letdown reflex) when nursing | |
| Vasopressin (antidiuretic hormone) | ADH or AVP | Parvocellular neurosecretory neurons | Increases water permeability in the distal convoluted tubule and collecting duct of nephrons, thus promoting water reabsorption and increasing blood volume |
Oxytocin and anti-diuretic hormone are not secreted in the posterior lobe, merely stored.
Thyroid
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Triiodothyronine | T3 | Thyroid epithelial cell | (More potent form of thyroid hormone) Stimulates body oxygen and energy consumption, thereby increasing the basal metabolic rate Stimulates RNA polymerase I and II, thereby promoting protein synthesis |
| Thyroxine (tetraiodothyronine) | T4 | Thyroid epithelial cells | (Less active form of thyroid hormone) (Acts as a prohormone to triiodothyronine) Stimulates body oxygen and energy consumption, thereby increasing the basal metabolic rate Stimulates RNA polymerase I and II, thereby promoting protein synthesis |
| Calcitonin | Parafollicular cells | Stimulates osteoblasts and thus bone construction Inhibits Ca2+ release from bone, thereby reducing blood Ca2+ |
Alimentary system
Stomach
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Gastrin (Primarily) | G cells | Secretion of gastric acid by parietal cells | |
| Ghrelin | P/D1 cells | Stimulate appetite,
secretion of growth hormone from anterior pituitary gland
| |
| Neuropeptide Y | NPY | increased food intake and decreased physical activity. It can be associated with obesity. | |
| Somatostatin | D cells | Suppress release of gastrin, cholecystokinin (CCK),secretin, motilin, vasoactive intestinal peptide (VIP),gastric inhibitory polypeptide (GIP), enteroglucagon
Lowers rate of gastric emptying
Reduces smooth muscle contractions and blood flow within the intestine.[1]
| |
| Histamine | ECL cells | stimulate gastric acid secretion | |
| Endothelin | X cells | Smooth muscle contraction of stomach[2] |
Duodenum (small intestine)[edit]
| Secreted hormone | From cells | Effect |
|---|---|---|
| Secretin | S cells | Secretion of bicarbonate from liver, pancreas and duodenalBrunner's glands
Enhances effects of cholecystokinin, stops production of gastric juice
|
| Cholecystokinin | I cells | Release of digestive enzymes from pancreas |
Liver
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Insulin-like growth factor(or somatomedin) (Primarily) | IGF | Hepatocytes | insulin-like effects
regulate cell growth and development
|
| Angiotensinogen andangiotensin | Hepatocytes | vasoconstriction | |
| Thrombopoietin | THPO | Hepatocytes | stimulates megakaryocytes to produce platelets[3] |
| Hepcidin | Hepatocytes | inhibits intestinal iron absorption and iron release bymacrophages |
Pancreas
Pancreas is a mixed endocrine and exocrine gland and it secretes both enzymes and hormones.
| Secreted hormone | From cells | Effect |
|---|---|---|
| Insulin (Primarily) | β Islet cells | Intake of glucose, glycogenesis and glycolysis in liver andmuscle from blood |
| Glucagon (Also Primarily) | α Islet cells | glycogenolysis and gluconeogenesis in liver
increases blood glucose level
|
| Somatostatin | δ Islet cells | Inhibit release of insulin[4] |
| Pancreatic polypeptide | PP cells | Self regulate the pancreas secretion activities and effect the hepatic glycogen levels. |
Kidney
| Secreted hormone | From cells | Effect |
|---|---|---|
| Renin (Primarily) | Juxtaglomerular cells | Activates the renin-angiotensin system by producingangiotensin I of angiotensinogen |
| Erythropoietin (EPO) | Extraglomerular mesangial cells | Stimulate erythrocyte production |
| Calcitriol (1,25-dihydroxyvitamin D3) | Active form of vitamin D3
Increase absorption of calcium and phosphate fromgastrointestinal tract and kidneys inhibit release of PTH
| |
| Thrombopoietin | stimulates megakaryocytes to produce platelets[3] |
Adrenal glands
Adrenal cortex
| Secreted hormone | From cells | Effect |
|---|---|---|
| Glucocorticoids (chieflycortisol) | zona fasciculata and zona reticularis cells | Stimulates gluconeogenesis Stimulates fat breakdown in adipose tissue Inhibits protein synthesis Inhibits glucose uptake in muscle and adipose tissue Inhibits immunological responses (immunosuppressive) Inhibits inflammatory responses (anti-inflammatory) |
| Mineralocorticoids(chiefly aldosterone) | Zona glomerulosa cells | Stimulates active sodium reabsorption in kidneys Stimulates passive water reabsorption in kidneys, thus increasing blood volume and blood pressure Stimulates potassium and H+ secretion into nephron of kidney and subsequent excretion |
| Androgens (includingDHEA and testosterone) | Zona fasciculata and Zona reticularis cells | In males: Relatively small effect compared to androgens from testes In females: masculinizing effects |
Adrenal medulla
| Secreted hormone | From cells | Effect |
|---|---|---|
| Adrenaline (epinephrine) (Primarily) | Chromaffin cells | Fight-or-flight response:
|
| Noradrenaline(norepinephrine) | Chromaffin cells | Fight-or-flight response:
|
| Dopamine | Chromaffin cells | Increase heart rate and blood pressure |
| Enkephalin | Chromaffin cells | Regulate pain |
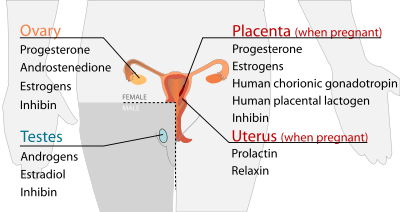
Reproductive
Testes
| Secreted hormone | From cells | Effect |
|---|---|---|
| Androgens (chieflytestosterone) | Leydig cells | Anabolic: growth of muscle mass and strength, increasedbone density, growth and strength,
Virilizing: maturation of sex organs, formation of scrotum, deepening of voice, growth of beard and axillary hair.
|
| Estradiol | Sertoli cells | Prevent apoptosis of germ cells[5] |
| Inhibin | Sertoli cells | Inhibit production of FSH |
Ovarian follicle and corpus luteum
| Secreted hormone | From cells | Effect |
|---|---|---|
| Progesterone | Granulosa cells, theca cells | Support pregnancy:[6]
Other:
|
| Androstenedione | Theca cells | Substrate for estrogen |
| Estrogens (mainlyestradiol) | Granulosa cells | Structural:
Protein synthesis:
Fluid balance:
Gastrointestinal tract:
Melanin:
Cancer:
Lung function:
|
| Inhibin | Granulosa cells | Inhibit production of FSH from anterior pituitary |
Placenta (when pregnant)
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Progesterone (Primarily) | Support pregnancy:[6]
Other effects on mother similar to ovarian follicle-progesterone
| ||
| Estrogens (mainly Estriol) (Also Primarily) | Effects on mother similar to ovarian follicle estrogen | ||
| Human chorionic gonadotropin | HCG | Syncytiotrophoblast | Promote maintenance of corpus luteum during beginning of pregnancy
Inhibit immune response, towards the human embryo.
|
| Human placental lactogen | HPL | Syncytiotrophoblast | Increase production of insulin and IGF-1
Increase insulin resistance and carbohydrateintolerance
|
| Inhibin | Fetal Trophoblasts | Suppress FSH |
Uterus (when pregnant)
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Prolactin | PRL | Decidual cells | milk production in mammary glands |
| Relaxin | Decidual cells | Unclear in humans and animals |
Calcium regulation
Further information: Calcium metabolism
Parathyroid
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Parathyroid hormone | PTH | Parathyroid chief cell | Calcium:
|
Skin
| Secreted hormone | From cells | Effect |
|---|---|---|
| Calcidiol (25-hydroxyvitamin D3) | Inactive form of vitamin D3 |
Targets
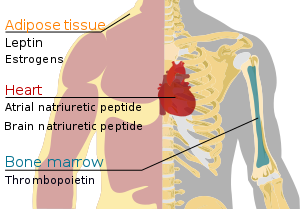
Heart
| Secreted hormone | Abbreviation | From cells | Effect |
|---|---|---|---|
| Atrial-natriuretic peptide | ANP | Cardiac myocytes | Reduce blood pressure by: |
| Brain natriuretic peptide | BNP | Cardiac myocytes | (To a lesser degree than ANP) reduce blood pressureby: |
Bone marrow[edit]
| Secreted hormone | From cells | Effect |
|---|---|---|
| Thrombopoietin | liver and kidney cells | stimulates megakaryocytes to produce platelets[3] |
Skeletal muscle
In 1998, skeletal muscle was identified as an endocrine organ[11] due to its now well-established role in the secretion ofmyokines.[11][12] The use of the term myokine to describe cytokines and other peptides produced by muscle as signalling molecules was proposed in 2003.[13]
Adipose tissue
Signalling molecules released by adipose tissue are referred to as adipokines.
| Secreted hormone | From cells | Effect |
|---|---|---|
| Leptin (Primarily) | Adipocytes | decrease of appetite and increase of metabolism. |
| Estrogens[14] (mainlyEstrone) | Adipocytes |
Diffuse neuro-endocrine system (DNES)[edit]
The Diffuse neuro-endocrine system (DNES) comprises hormone-secreted cells, that have commonalities with neurons and are found in the Epithelium of organs of the body.
Major endocrine systems
The human endocrine system consists of several systems that operate via feedback loops. Several important feedback systems are mediated via the hypothalamus and pituitary.[15]
- TRH – TSH – T3/T4
- GnRH – LH/FSH – sex hormones
- CRH – ACTH – cortisol
- Renin – angiotensin – aldosterone
- leptin vs. insulin
Interaction with immune system[edit]
Extensive bidirectional interactions exist between the endocrine system and the immune system.[16] Cortisol has majorimmunosuppressive effects,[17][18] and dopamine has immunomodulatory functions.[19] On the other hand, cytokinesproduced during inflammation activate the HPA axis at all three levels, sensible to negative feedback.[20] Moreover cytokines stimulate hepcidin release from the liver, which is eventually responsible for the anemia of chronic disease.[21]
In other species
A neuroendocrine system has been observed in all animals with a nervous system and all vertebrates have an hypothalamus-pituitary axis.[22] All vertebrates have a thyroid, which in amphibians is also crucial for transformation of larvae into adult form.[23][24] All vertebrates have adrenal gland tissue, with mammals unique in having it organized into layers.[25] All vertebrates have some form of renin-angiotensin axis, and all tetrapods have aldosterone as primarymineralocorticoid.[26][27]
Diseases
Main article: Endocrine diseases
Diseases of the endocrine system are common,[29] including conditions such asdiabetes mellitus, thyroid disease, and obesity. Endocrine disease is characterized by disregulated hormone release (a productive pituitary adenoma), inappropriate response to signaling (hypothyroidism), lack of a gland (diabetes mellitus type 1, diminished erythropoiesis in chronic renal failure), or structural enlargement in a critical site such as the thyroid (toxic multinodular goitre). Hypofunction of endocrine glands can occur as a result of loss of reserve, hyposecretion, agenesis, atrophy, or active destruction. Hyperfunction can occur as a result of hypersecretion, loss of suppression, hyperplastic or neoplastic change, or hyperstimulation.
Endocrinopathies are classified as primary, secondary, or tertiary. Primary endocrine disease inhibits the action of downstream glands. Secondary endocrine disease is indicative of a problem with the pituitary gland. Tertiary endocrine disease is associated with dysfunction of the hypothalamus and its releasing hormones.[citation needed]
As the thyroid, and hormones have been implicated in signaling distant tissues to proliferate, for example, the estrogen receptor has been shown to be involved in certain breast cancers. Endocrine, paracrine, and autocrine signaling have all been implicated in proliferation, one of the required steps of oncogenesis.[30]
Other types of signaling
The typical mode of cell signaling in the endocrine system is endocrine signaling. However, there are also other modes, i.e., paracrine, autocrine, and neuroendocrine signaling. Purely neurocrine signaling between neurons, on the other hand, belongs completely to the nervous system.
Autocrine
Main article: Autocrine signalling
Autocrine signaling is a form of signaling in which a cell secretes a hormone or chemical messenger (called the autocrine agent) that binds to autocrine receptors on the same cell, leading to changes in the cells.
Paracrine
Main article: Paracrine signalling
Paracrine signaling is a form of cell signaling in which the target cell is near the signal-releasing cell, altering the behavior or differentiation of those competent cells.
Juxtacrine
Main article: Juxtacrine signalling
Juxtacrine signaling is a type of intercellular communication that is transmitted via oligosaccharide, lipid, or protein components of a cell membrane, and may affect either the emitting cell or the immediately adjacent cells.
It occurs between adjacent cells that possess broad patches of closely opposed plasma membrane linked by transmembrane channels known as connexons. The gap between the cells can usually be between only 2 and 4 nm.
Unlike other types of cell signaling (such as paracrine and endocrine), juxtacrine signaling requires physical contact between the two cells involved.
Juxtacrine signaling has been observed for some growth factors, cytokine and chemokine cellular signals.
Additional images
Hormone
A hormone (from Greek ὁρμή, "impetus") is any member of a class of signaling molecules produced by glands in multicellular organisms that are transported by thecirculatory system to target distant organs to regulate physiology and behaviour. Hormones have diverse chemical structures that include eicosanoids, steroids, amino acid derivatives, peptides, and proteins. The glands that secrete hormones comprise the endocrine signaling system. The term hormone is sometimes extended to include chemicals produced by cells that affect the same cell (autocrine orintracrine signalling) or nearby cells (paracrine signalling).
Hormones are used to communicate between organs and tissues to regulate physiological and behavioral activities, such as digestion, metabolism, respiration,tissue function, sensory perception, sleep, excretion, lactation, stress, growth and development, movement, reproduction, and mood.[1][2] Hormones affect distant cells by binding to specific receptor proteins in the target cell resulting in a change in cell function. When a hormone binds to the receptor, it results in the activation of asignal transduction pathway. This may lead to cell type-specific responses that include rapid non-genomic effects or slower genomic responses where the hormones acting through their receptors activate gene transcription resulting in increased expression of target proteins.
Hormone synthesis may occur in specific tissues of endocrine glands or in other specialized cells. Hormone synthesis occurs in response to specific biochemical signals induced by a wide range of regulatory systems. For instance, ionized calcium concentration affects PTH synthesis, whereas glucose concentration affects insulin synthesis. Regulation of hormone synthesis of gonadal, adrenal, and thyroid hormones is often dependent on complex sets of direct influence and feedback interactions involving the hypothalamic-pituitary-adrenal (HPA), -gonadal (HPG), and -thyroid (HPT) axes.
Upon secretion, certain hormones, including protein hormones and catecholamines, are water-soluble and are thus readily transported through the circulatory system. Other hormones, including steroid and thyroid hormones, are lipid-soluble; to allow for their widespread distribution, these hormones must bond to carrier plasma glycoproteins (e.g., thyroxine-binding globulin (TBG)) to form ligand-protein complexes. Some hormones are completely active when released into the bloodstream (as is the case for insulin and growth hormones), while others must be activated in specific cells through a series of activation steps that are commonly highly regulated. The endocrine system secretes hormones directly into thebloodstream typically into fenestrated capillaries, whereas the exocrine system secretes its hormones indirectly using ducts. Hormones with paracrine function diffuse through the interstitial spaces to nearby target tissue.
A hormone (from Greek ὁρμή, "impetus") is any member of a class of signaling molecules produced by glands in multicellular organisms that are transported by thecirculatory system to target distant organs to regulate physiology and behaviour. Hormones have diverse chemical structures that include eicosanoids, steroids, amino acid derivatives, peptides, and proteins. The glands that secrete hormones comprise the endocrine signaling system. The term hormone is sometimes extended to include chemicals produced by cells that affect the same cell (autocrine orintracrine signalling) or nearby cells (paracrine signalling).
Hormones are used to communicate between organs and tissues to regulate physiological and behavioral activities, such as digestion, metabolism, respiration,tissue function, sensory perception, sleep, excretion, lactation, stress, growth and development, movement, reproduction, and mood.[1][2] Hormones affect distant cells by binding to specific receptor proteins in the target cell resulting in a change in cell function. When a hormone binds to the receptor, it results in the activation of asignal transduction pathway. This may lead to cell type-specific responses that include rapid non-genomic effects or slower genomic responses where the hormones acting through their receptors activate gene transcription resulting in increased expression of target proteins.
Hormone synthesis may occur in specific tissues of endocrine glands or in other specialized cells. Hormone synthesis occurs in response to specific biochemical signals induced by a wide range of regulatory systems. For instance, ionized calcium concentration affects PTH synthesis, whereas glucose concentration affects insulin synthesis. Regulation of hormone synthesis of gonadal, adrenal, and thyroid hormones is often dependent on complex sets of direct influence and feedback interactions involving the hypothalamic-pituitary-adrenal (HPA), -gonadal (HPG), and -thyroid (HPT) axes.
Upon secretion, certain hormones, including protein hormones and catecholamines, are water-soluble and are thus readily transported through the circulatory system. Other hormones, including steroid and thyroid hormones, are lipid-soluble; to allow for their widespread distribution, these hormones must bond to carrier plasma glycoproteins (e.g., thyroxine-binding globulin (TBG)) to form ligand-protein complexes. Some hormones are completely active when released into the bloodstream (as is the case for insulin and growth hormones), while others must be activated in specific cells through a series of activation steps that are commonly highly regulated. The endocrine system secretes hormones directly into thebloodstream typically into fenestrated capillaries, whereas the exocrine system secretes its hormones indirectly using ducts. Hormones with paracrine function diffuse through the interstitial spaces to nearby target tissue.
Contents
Overview
Further information: Signal transduction
Hormonal signaling involves the following steps:[3]
- Biosynthesis of a particular hormone in a particular tissue
- Storage and secretion of the hormone
- Transport of the hormone to the target cell(s)
- Recognition of the hormone by an associated cell membrane or intracellular receptor protein
- Relay and amplification of the received hormonal signal via a signal transduction process: This then leads to a cellular response. The reaction of the target cells may then be recognized by the original hormone-producing cells, leading to a down-regulation in hormone production. This is an example of a homeostatic negative feedback loop.
- Breakdown of the hormone.
Hormone cells are typically of a specialized cell type, residing within a particular endocrine gland, such as the thyroid gland,ovaries, and testes. Hormones exit their cell of origin via exocytosis or another means of membrane transport. The hierarchical model is an oversimplification of the hormonal signaling process. Cellular recipients of a particular hormonal signal may be one of several cell types that reside within a number of different tissues, as is the case for insulin, which triggers a diverse range of systemic physiological effects. Different tissue types may also respond differently to the same hormonal signal.
Further information: Signal transduction
Hormonal signaling involves the following steps:[3]
- Biosynthesis of a particular hormone in a particular tissue
- Storage and secretion of the hormone
- Transport of the hormone to the target cell(s)
- Recognition of the hormone by an associated cell membrane or intracellular receptor protein
- Relay and amplification of the received hormonal signal via a signal transduction process: This then leads to a cellular response. The reaction of the target cells may then be recognized by the original hormone-producing cells, leading to a down-regulation in hormone production. This is an example of a homeostatic negative feedback loop.
- Breakdown of the hormone.
Hormone cells are typically of a specialized cell type, residing within a particular endocrine gland, such as the thyroid gland,ovaries, and testes. Hormones exit their cell of origin via exocytosis or another means of membrane transport. The hierarchical model is an oversimplification of the hormonal signaling process. Cellular recipients of a particular hormonal signal may be one of several cell types that reside within a number of different tissues, as is the case for insulin, which triggers a diverse range of systemic physiological effects. Different tissue types may also respond differently to the same hormonal signal.
Regulation
The rate of hormone biosynthesis and secretion is often regulated by a homeostatic negative feedback control mechanism. Such a mechanism depends on factors that influence the metabolism and excretion of hormones. Thus, higher hormone concentration alone cannot trigger the negative feedback mechanism. Negative feedback must be triggered by overproduction of an "effect" of the hormone.
Hormone secretion can be stimulated and inhibited by:
- Other hormones (stimulating- or releasing -hormones)
- Plasma concentrations of ions or nutrients, as well as binding globulins
- Neurons and mental activity
- Environmental changes, e.g., of light or temperature
One special group of hormones is the tropic hormones that stimulate the hormone production of other endocrine glands. For example, thyroid-stimulating hormone (TSH) causes growth and increased activity of another endocrine gland, the thyroid, which increases output of thyroid hormones.
To release active hormones quickly into the circulation, hormone biosynthetic cells may produce and store biologically inactive hormones in the form of pre- or prohormones. These can then be quickly converted into their active hormone form in response to a particular stimulus.
Eicosanoids are considered to act as local hormones.
The rate of hormone biosynthesis and secretion is often regulated by a homeostatic negative feedback control mechanism. Such a mechanism depends on factors that influence the metabolism and excretion of hormones. Thus, higher hormone concentration alone cannot trigger the negative feedback mechanism. Negative feedback must be triggered by overproduction of an "effect" of the hormone.
Hormone secretion can be stimulated and inhibited by:
- Other hormones (stimulating- or releasing -hormones)
- Plasma concentrations of ions or nutrients, as well as binding globulins
- Neurons and mental activity
- Environmental changes, e.g., of light or temperature
One special group of hormones is the tropic hormones that stimulate the hormone production of other endocrine glands. For example, thyroid-stimulating hormone (TSH) causes growth and increased activity of another endocrine gland, the thyroid, which increases output of thyroid hormones.
To release active hormones quickly into the circulation, hormone biosynthetic cells may produce and store biologically inactive hormones in the form of pre- or prohormones. These can then be quickly converted into their active hormone form in response to a particular stimulus.
Eicosanoids are considered to act as local hormones.
Receptors
Most hormones initiate a cellular response by initially binding to either cell membrane associated orintracellular receptors. A cell may have several different receptor types that recognize the same hormone but activate different signal transduction pathways, or a cell may have several different receptors that recognize different hormones and activate the same biochemical pathway.
Receptors for most peptide as well as many eicosanoidhormones are embedded in the plasma membrane at the surface of the cell and the majority of these receptors belong to the G protein-coupled receptor(GPCR) class of seven alpha helix transmembraneproteins. The interaction of hormone and receptor typically triggers a cascade of secondary effects within the cytoplasm of the cell, often involving phosphorylation or dephosphorylation of various other cytoplasmic proteins, changes in ion channel permeability, or increased concentrations of intracellular molecules that may act as secondary messengers (e.g., cyclic AMP). Some protein hormones also interact with intracellular receptors located in the cytoplasm or nucleus by an intracrine mechanism.
For steroid or thyroid hormones, their receptors are located inside the cell within the cytoplasm of the target cell. These receptors belong to the nuclear receptor family of ligand-activated transcription factors. To bind their receptors, these hormones must first cross the cell membrane. They can do so because they are lipid-soluble. The combined hormone-receptor complex then moves across the nuclear membrane into the nucleus of the cell, where it binds to specific DNA sequences, regulating the expression of certain genes, and thereby increasing the levels of the proteins encoded by these genes.[4] However, it has been shown that not all steroid receptors are located inside the cell. Some are associated with theplasma membrane.[5]
Most hormones initiate a cellular response by initially binding to either cell membrane associated orintracellular receptors. A cell may have several different receptor types that recognize the same hormone but activate different signal transduction pathways, or a cell may have several different receptors that recognize different hormones and activate the same biochemical pathway.
Receptors for most peptide as well as many eicosanoidhormones are embedded in the plasma membrane at the surface of the cell and the majority of these receptors belong to the G protein-coupled receptor(GPCR) class of seven alpha helix transmembraneproteins. The interaction of hormone and receptor typically triggers a cascade of secondary effects within the cytoplasm of the cell, often involving phosphorylation or dephosphorylation of various other cytoplasmic proteins, changes in ion channel permeability, or increased concentrations of intracellular molecules that may act as secondary messengers (e.g., cyclic AMP). Some protein hormones also interact with intracellular receptors located in the cytoplasm or nucleus by an intracrine mechanism.
For steroid or thyroid hormones, their receptors are located inside the cell within the cytoplasm of the target cell. These receptors belong to the nuclear receptor family of ligand-activated transcription factors. To bind their receptors, these hormones must first cross the cell membrane. They can do so because they are lipid-soluble. The combined hormone-receptor complex then moves across the nuclear membrane into the nucleus of the cell, where it binds to specific DNA sequences, regulating the expression of certain genes, and thereby increasing the levels of the proteins encoded by these genes.[4] However, it has been shown that not all steroid receptors are located inside the cell. Some are associated with theplasma membrane.[5]
Effects
A variety of exogenous chemical compounds, both natural and synthetic, have hormone-like effects on both humans and wildlife. Their interference with the synthesis, secretion, transport, binding, action, or elimination of natural hormones in the body can change the homeostasis, reproduction, development, and/or behavior, similar to endogenously produced hormones.[6]
Hormones have the following effects on the body:
- stimulation or inhibition of growth
- wake-sleep cycle and other circadian rhythms
- mood swings
- induction or suppression of apoptosis (programmed cell death)
- activation or inhibition of the immune system
- regulation of metabolism
- preparation of the body for mating, fighting, fleeing, and other activity
- preparation of the body for a new phase of life, such as puberty, parenting, and menopause
- control of the reproductive cycle
- hunger cravings
- sexual arousal
A hormone may also regulate the production and release of other hormones. Hormone signals control the internal environment of the body through homeostasis.
A variety of exogenous chemical compounds, both natural and synthetic, have hormone-like effects on both humans and wildlife. Their interference with the synthesis, secretion, transport, binding, action, or elimination of natural hormones in the body can change the homeostasis, reproduction, development, and/or behavior, similar to endogenously produced hormones.[6]
Hormones have the following effects on the body:
- stimulation or inhibition of growth
- wake-sleep cycle and other circadian rhythms
- mood swings
- induction or suppression of apoptosis (programmed cell death)
- activation or inhibition of the immune system
- regulation of metabolism
- preparation of the body for mating, fighting, fleeing, and other activity
- preparation of the body for a new phase of life, such as puberty, parenting, and menopause
- control of the reproductive cycle
- hunger cravings
- sexual arousal
A hormone may also regulate the production and release of other hormones. Hormone signals control the internal environment of the body through homeostasis.
Chemical classes
As hormones are defined functionally, not structurally, they may have diverse chemical structures. Hormones occur inmulticellular organisms (plants, animals, fungi, brown algae and red algae). These compounds occur also in unicellular organisms, and may act as signaling molecules,[7][8] but there is no consensus if, in this case, they can be called hormones.
As hormones are defined functionally, not structurally, they may have diverse chemical structures. Hormones occur inmulticellular organisms (plants, animals, fungi, brown algae and red algae). These compounds occur also in unicellular organisms, and may act as signaling molecules,[7][8] but there is no consensus if, in this case, they can be called hormones.
Animal
Further information: List of human hormones
Vertebrate hormones fall into four main chemical classes:
- Amino acid derived – Examples include melatonin and thyroxine.
- Polypeptide and proteins. – Small peptide hormones include TRH and vasopressin. Peptides composed of scores or hundreds of amino acids are referred to as proteins. Examples of protein hormones include insulin and growth hormone. More complex protein hormones bear carbohydrate side-chains and are called glycoprotein hormones. Luteinizing hormone, follicle-stimulating hormone and thyroid-stimulating hormone are examples of glycoprotein hormones.
- Eicosanoids – hormones derive from lipids such as arachidonic acid, lipoxins and prostaglandins.
- Steroid – Examples of steroid hormones include the sex hormones estradiol and testosterone as well as the stress hormone cortisol.
Compared with vertebrate, insects and crustaceans possess a number of structurally unusual hormones such as thejuvenile hormone, a sesquiterpenoid.[9]
Further information: List of human hormones
Vertebrate hormones fall into four main chemical classes:
- Amino acid derived – Examples include melatonin and thyroxine.
- Polypeptide and proteins. – Small peptide hormones include TRH and vasopressin. Peptides composed of scores or hundreds of amino acids are referred to as proteins. Examples of protein hormones include insulin and growth hormone. More complex protein hormones bear carbohydrate side-chains and are called glycoprotein hormones. Luteinizing hormone, follicle-stimulating hormone and thyroid-stimulating hormone are examples of glycoprotein hormones.
- Eicosanoids – hormones derive from lipids such as arachidonic acid, lipoxins and prostaglandins.
- Steroid – Examples of steroid hormones include the sex hormones estradiol and testosterone as well as the stress hormone cortisol.
Compared with vertebrate, insects and crustaceans possess a number of structurally unusual hormones such as thejuvenile hormone, a sesquiterpenoid.[9]
Plant
Further information: Plant hormone § Classes of plant hormones
Further information: Plant hormone § Classes of plant hormones
Therapeutic use
Many hormones and their analogues are used as medication. The most commonly prescribed hormones are estrogens andprogestogens (as methods of hormonal contraception and as HRT), thyroxine (as levothyroxine, for hypothyroidism) andsteroids (for autoimmune diseases and several respiratory disorders). Insulin is used by many diabetics. Local preparations for use in otolaryngology often contain pharmacologic equivalents of adrenaline, while steroid and vitamin D creams are used extensively in dermatological practice.
A "pharmacologic dose" or "supraphysiological dose" of a hormone is a medical usage referring to an amount of a hormone far greater than naturally occurs in a healthy body. The effects of pharmacologic doses of hormones may be different from responses to naturally occurring amounts and may be therapeutically useful, though not without potentially adverse side effects. An example is the ability of pharmacologic doses of glucocorticoids to suppress inflammation.
Many hormones and their analogues are used as medication. The most commonly prescribed hormones are estrogens andprogestogens (as methods of hormonal contraception and as HRT), thyroxine (as levothyroxine, for hypothyroidism) andsteroids (for autoimmune diseases and several respiratory disorders). Insulin is used by many diabetics. Local preparations for use in otolaryngology often contain pharmacologic equivalents of adrenaline, while steroid and vitamin D creams are used extensively in dermatological practice.
A "pharmacologic dose" or "supraphysiological dose" of a hormone is a medical usage referring to an amount of a hormone far greater than naturally occurs in a healthy body. The effects of pharmacologic doses of hormones may be different from responses to naturally occurring amounts and may be therapeutically useful, though not without potentially adverse side effects. An example is the ability of pharmacologic doses of glucocorticoids to suppress inflammation.
Hormone-behavior interactions
T
At the neurological level, behavior can be inferred based on: hormone concentrations; hormone-release patterns; the numbers and locations of hormone receptors; and the efficiency of hormone receptors for those involved in gene transcription. Not only do hormones influence behavior, but also behavior and the environment influence hormones. Thus, a feedback loop is formed. For example, behavior can affect hormones, which in turn can affect behavior, which in turn can affect hormones, and so on.
Three broad stages of reasoning may be used when determining hormone-behavior interactions:
- The frequency of occurrence of a hormonally dependent behavior should correspond to that of its hormonal source
- A hormonally dependent behavior is not expected if the hormonal source (or its types of action) is non-existent
- The reintroduction of a missing behaviorally dependent hormonal source (or its types of action) is expected to bring back the absent behavior
| T |
At the neurological level, behavior can be inferred based on: hormone concentrations; hormone-release patterns; the numbers and locations of hormone receptors; and the efficiency of hormone receptors for those involved in gene transcription. Not only do hormones influence behavior, but also behavior and the environment influence hormones. Thus, a feedback loop is formed. For example, behavior can affect hormones, which in turn can affect behavior, which in turn can affect hormones, and so on.
Three broad stages of reasoning may be used when determining hormone-behavior interactions:
- The frequency of occurrence of a hormonally dependent behavior should correspond to that of its hormonal source
- A hormonally dependent behavior is not expected if the hormonal source (or its types of action) is non-existent
- The reintroduction of a missing behaviorally dependent hormonal source (or its types of action) is expected to bring back the absent behavior
Comparison with neurotransmitters
There are various clear distinctions between hormones and neurotransmitters:
- A hormone can perform functions over a larger spatial and temporal scale than can a neurotransmitter.
- Hormonal signals can travel virtually anywhere in the circulatory system, whereas neural signals are restricted to pre-existing nerve tracts
- Assuming the travel distance is equivalent, neural signals can be transmitted much more quickly (in the range of milliseconds) than can hormonal signals (in the range of seconds, minutes, or hours). Neural signals can be sent at speeds up to 100 meters per second.
- Neural signaling is an all-or-nothing (digital) action, whereas hormonal signaling is an action that can be continuously variable as dependent upon hormone concentration
There are various clear distinctions between hormones and neurotransmitters:
- A hormone can perform functions over a larger spatial and temporal scale than can a neurotransmitter.
- Hormonal signals can travel virtually anywhere in the circulatory system, whereas neural signals are restricted to pre-existing nerve tracts
- Assuming the travel distance is equivalent, neural signals can be transmitted much more quickly (in the range of milliseconds) than can hormonal signals (in the range of seconds, minutes, or hours). Neural signals can be sent at speeds up to 100 meters per second.
- Neural signaling is an all-or-nothing (digital) action, whereas hormonal signaling is an action that can be continuously variable as dependent upon hormone concentration








No comments:
Post a Comment