Exocrine gland
| Exocrine gland | |
|---|---|
| Details | |
| Latin | glandula exocrina |
| Anatomical terminology | |
Exocrine glands are glands of the exocrine system that secrete their essential product by way of a duct to some environment external to itself, either inside the body or on a surface of the body. Exocrine glands are one of two types of glands in the human body, the other being endocrine glands, which secrete their products directly into the bloodstream. Examples of exocrine glands include sweat, salivary, mammary, ceruminous, lacrimal, sebaceous, and mucous. The liver and pancreas are both exocrine and endocrine gland; they are exocrine glands because they secrete by way of the hepatic and pancreatic ducts.
Contents
[hide]Classification
By structure
Exocrine glands contain a glandular portion and a duct portion, the structures of which can be used to classify the gland.
- The duct portion may be branched (called compound) or unbranched (called simple).
- The glandular portion may be tubular or acinar, or may be a mix of the two (called tubuloacinar). If the glandular portion branches, then the gland is called a branched gland.
By method of excretion
Exocrine glands are named apocrine glands, holocrine glands, or merocrine glands based on how their products are excreted.
- Merocrine secretion - cells excrete their substances by exocytosis; for example, pancreatic acinar cells.
- Apocrine secretion - a portion of the plasma membrane buds off the cell, containing the excretion.
- Holocrine secretion - the entire cell disintegrates to excrete its substance; for example, sebaceous glands of the skin and nose.
By product excreted
- Serous cells excrete proteins, often enzymes. Examples include gastric chief cells and Paneth cells
- Mucous cells excrete mucus. Examples include Brunner's glands, esophageal glands, and pyloric glands
- Mixed glands excrete both protein and mucus. Examples include the salivary glands, although the parotid gland is predominantly serous, the sublingual gland is predominantly mucous, and the submandibular gland is both serous and mucous.
Human skin
| Skin | |
|---|---|

| |
| Details | |
| Latin | cutis |
| Anatomical terminology | |
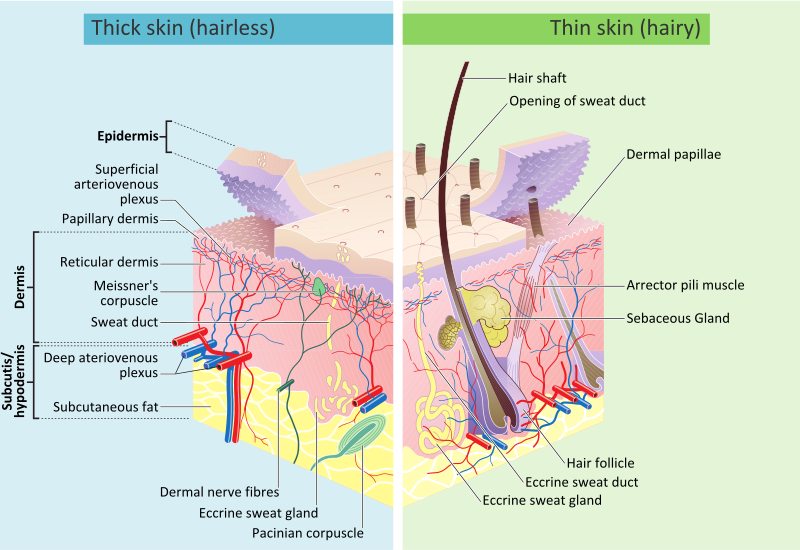
The human skin is the outer covering of the body. In humans, it is the largest organ of the integumentary system. The skin has multiple layers of ectodermaltissue and guards the underlying muscles, bones, ligaments and internal organs.[1] Human skin is similar to that of most other mammals, except that it is not protected by a fur. Though nearly all human skin is covered with hair follicles, it can appear hairless. There are two general types of skin, hairy andglabrous skin.[2] The adjective cutaneous literally means "of the skin" (from Latin cutis, skin).
Because it interfaces with the environment, skin plays a key immunity role in protecting the body against pathogens[3] and excessive water loss.[4] Its other functions are insulation, temperature regulation, sensation, synthesis of vitamin D, and the protection of vitamin B folates. Severely damaged skin will try to heal by forming scar tissue. This is often discolored and depigmented.
In humans, skin pigmentation varies among populations, and skin type can range from dry to oily. Such skin variety provides a rich and diverse habitat forbacteria that number roughly 1000 species from 19 phyla.[5][6]
Skin components
See also: Skin layers
Skin has mesodermal cells, pigmentation, or melanin provided by melanocytes, which absorb some of the potentially dangerous ultraviolet radiation (UV) in sunlight. It also contains DNA repair enzymes that help reverse UV damage, such that people lacking the genes for these enzymes suffer high rates of skin cancer. One form predominantly produced by UV light,malignant melanoma, is particularly invasive, causing it to spread quickly, and can often be deadly. Human skin pigmentation varies among populations in a striking manner. This has led to the classification of people(s) on the basis of skin color.[7]
The skin is the largest organ in the human body. For the average adult human, the skin has a surface area of between 1.5-2.0 square metres (16.1-21.5 sq ft.), most of it between 2–3 mm (0.10 inch) thick. The average square inch (6.5 cm²) of skin holds 650 sweat glands, 20 blood vessels, 60,000 melanocytes, and more than 1,000 nerve endings.[8]
Functions
Skin performs the following functions:
- Protection: an anatomical barrier from pathogens and damage between the internal and external environment in bodily defense; Langerhans cells in the skin are part of the adaptive immune system.[3][4]
- Sensation: contains a variety of nerve endings that react to heat and cold, touch, pressure, vibration, and tissue injury; see somatosensory system and haptics.
- Heat regulation: the skin contains a blood supply far greater than its requirements which allows precise control of energy loss by radiation, convection and conduction. Dilated blood vessels increase perfusion and heatloss, while constricted vessels greatly reduce cutaneous blood flow and conserve heat.
- Control of evaporation: the skin provides a relatively dry and semi-impermeable barrier to fluid loss.[4] Loss of this function contributes to the massive fluid loss in burns.
- Aesthetics and communication: others see our skin and can assess our mood, physical state and attractiveness.
- Storage and synthesis: acts as a storage center for lipids and water, as well as a means of synthesis of vitamin Dby action of UV on certain parts of the skin.
- Excretion: sweat contains urea, however its concentration is 1/130th that of urine, hence excretion by sweating is at most a secondary function to temperature regulation.
- Absorption: the cells comprising the outermost 0.25–0.40 mm of the skin are "almost exclusively supplied by external oxygen", although the "contribution to total respiration is negligible".[9] In addition, medicine can be administered through the skin, by ointments or by means of adhesive patch, such as the nicotine patch oriontophoresis. The skin is an important site of transport in many other organisms.
- Water resistance: The skin acts as a water resistant barrier so essential nutrients aren't washed out of the body.
Pigments
There are at least five different pigments that determine the color of the skin.[10][11] These pigments are present at different levels and places.
- Melanin: It is brown in color and present in the germinative zone of the epidermis.
- Melanoid: It resembles melanin but is present diffusely throughout the epidermis.
- Carotene: This pigment is yellow to orange in color. It is present in the stratum corneum and fat cells of dermis and superficial fascia.
- Hemoglobin (also spelled haemoglobin): It is found in blood and is not a pigment of the skin but develops a purple color.
- Oxyhemoglobin: It is also found in blood and is not a pigment of the skin. It develops a red color.
See human skin color.
Hygiene and skin care
See also: Exfoliation (cosmetology)
The skin supports its own ecosystems of microorganisms, including yeasts and bacteria, which cannot be removed by any amount of cleaning. Estimates place the number of individual bacteria on the surface of one square inch (6.5 square cm) of human skin at 50 million, though this figure varies greatly over the average 20 square feet (1.9 m2) of human skin. Oily surfaces, such as the face, may contain over 500 million bacteria per square inch (6.5 cm²). Despite these vast quantities, all of the bacteria found on the skin's surface would fit into a volume the size of a pea.[12] In general, the microorganisms keep one another in check and are part of a healthy skin. When the balance is disturbed, there may be an overgrowth and infection, such as when antibiotics kill microbes, resulting in an overgrowth of yeast. The skin is continuous with the innerepithelial lining of the body at the orifices, each of which supports its own complement of microbes.
Cosmetics should be used carefully on the skin because these may cause allergic reactions. Each season requires suitable clothing in order to facilitate the evaporation of the sweat. Sunlight, water and air play an important role in keeping the skin healthy.
Oily skin
Oily skin is caused by over-active sebaceous glands, that produce a substance called sebum, a naturally healthy skin lubricant.[1] When the skin produces excessive sebum, it becomes heavy and thick in texture. Oily skin is typified by shininess, blemishes and pimples.[1] The oily-skin type is not necessarily bad, since such skin is less prone to wrinkling, or other signs of aging,[1] because the oil helps to keep needed moisture locked into the epidermis (outermost layer of skin).
The negative aspect of the oily-skin type is that oily complexions are especially susceptible to clogged pores, blackheads, and buildup of dead skin cells on the surface of the skin.[1] Oily skin can be sallow and rough in texture and tends to have large, clearly visible pores everywhere, except around the eyes and neck.[1]
Aging
For more details on this topic, see senescence.
For more details on this topic, see Intrinsic and extrinsic aging.
As skin ages, it becomes thinner and more easily damaged. Intensifying this effect is the decreasing ability of skin to heal itself as a person ages.
Among other things, skin aging is noted by a decrease in volume and elasticity. There are many internal and external causes to skin aging. For example, aging skin receives less blood flow and lower glandular activity.
A validated comprehensive grading scale has categorized the clinical findings of skin aging as laxity (sagging), rhytids (wrinkles), and the various facets of photoaging, including erythema/telangiectasia (redness), dyspigmentation (brown discoloration), solar elastosis (yellowing), keratoses (abnormal growths) and poor texture.[13]
Anti-aging supplements are used to treat skin aging.
Photoaging
Main article: Photoaging
Photoaging has two main concerns: an increased risk for skin cancer and the appearance of damaged skin. In younger skin, sun damage will heal faster since the cells in the epidermis have a faster turnover rate, while in the older population the skin becomes thinner and the epidermis turnover rate for cell repair is lower which may result in the dermis layer being damaged.[16]
Disease
For more details on this topic, see skin disease.
Diseases of the skin include skin infections and skin neoplasms (including skin cancer).
Variability in skin tone
Main article: Human skin color
Human skin shows high skin color variety from the darkest brown to the lightest pinkish-white hues. Human skin shows higher variation in color than any other single mammalian species and is the result of natural selection. Skin pigmentation in humans evolved to primarily regulate the amount of ultraviolet radiation (UVR) penetrating the skin, controlling its biochemical effects.[17]
The actual skin color of different humans is affected by many substances, although the single most important substance determining human skin color is the pigment melanin. Melanin is produced within the skin in cells called melanocytes and it is the main determinant of the skin color of darker-skinned humans. The skin color of people with light skin is determined mainly by the bluish-white connective tissue under the dermis and by the hemoglobin circulating in the veins of the dermis. The red color underlying the skin becomes more visible, especially in the face, when, as consequence of physical exerciseor the stimulation of the nervous system (anger, fear), arterioles dilate.[18]
There is a correlation between the geographic distribution of UV radiation (UVR) and the distribution of indigenous skin pigmentation around the world. Areas that highlight higher amounts of UVR reflect darker-skinned populations, generally located nearer towards the equator. Areas that are far from the tropics and closer to the poles have lower concentration of UVR, which is reflected in lighter-skinned populations.[19]
In the same population it has been observed that adult human females are considerably lighter in skin pigmentation thanmales. Females need more calcium during pregnancy and lactation and vitamin D which is synthesized from sunlight helps in absorbing calcium. For this reason it is thought that females may have evolved to have lighter skin in order to help their bodies absorb more calcium.[20]
| Description | ||
|---|---|---|
| I | Always burns, never tans | Pale, Fair, Freckles |
| II | Usually burns, sometimes tans | Fair |
| III | May burn, usually tans | Light Brown |
| IV | Rarely burns, always tans | Olive brown |
| V | Moderate constitutional pigmentation | Brown |
| VI | Marked constitutional pigmentation | Black |
Skin flora
Main article: Skin flora
The human skin is a rich environment for microbes.[5][6] Around 1000 species of bacteria from 19 bacterial phyla have been found. Most come from only four phyla: Actinobacteria (51.8%), Firmicutes (24.4%), Proteobacteria (16.5%), andBacteroidetes (6.3%). Propionibacteria and Staphylococci species were the main species in sebaceous areas. There are three main ecological areas: moist, dry and sebaceous. In moist places on the body Corynebacteria together withStaphylococci dominate. In dry areas, there is a mixture of species but dominated by b-Proteobacteria and Flavobacteriales. Ecologically, sebaceous areas had greater species richness than moist and dry ones. The areas with least similarity between people in species were the spaces between fingers, the spaces between toes, axillae, and umbilical cord stump. Most similarly were beside the nostril, nares (inside the nostril), and on the back.
Reflecting upon the diversity of the human skin researchers on the human skin microbiome have observed: "hairy, moist underarms lie a short distance from smooth dry forearms, but these two niches are likely as ecologically dissimilar as rainforests are to deserts."[5]
The NIH has been launched the Human Microbiome Project to characterize the human microbiota which includes that on the skin and the role of this microbiome in health and disease.[21]
Microorganisms like Staphylococcus epidermidis colonize the skin surface. The density of skin flora depends on region of the skin. The disinfected skin surface gets recolonized from bacteria residing in the deeper areas of the hair follicle, gut and urogenital openings.
Skin layers
Skin is composed of three primary layers:
- the epidermis, which provides waterproofing and serves as a barrier to infection;
- the dermis, which serves as a location for the appendages of skin; and
- the hypodermis (subcutaneous adipose layer).
Epidermis
Main article: Epidermis (skin)
Epidermis, "epi" coming from the Greek meaning "over" or "upon", is the outermost layer of the skin. It forms the waterproof, protective wrap over the body's surface and is made up of stratified squamous epithelium with an underlyingbasal lamina.
The epidermis contains no blood vessels, and cells in the deepest layers are nourished almost exclusively by diffused oxygen from the surrounding air[9] and to a far lesser degree by blood capillaries extending to the upper layers of the dermis. The main type of cells which make up the epidermis are Merkel cells, keratinocytes, with melanocytes andLangerhans cells also present. The epidermis can be further subdivided into the following strata (beginning with the outermost layer): corneum, lucidum (only in palms of hands and bottoms of feet), granulosum, spinosum, basale. Cells are formed through mitosis at the basale layer. The daughter cells (see cell division) move up the strata changing shape and composition as they die due to isolation from their blood source. The cytoplasm is released and the protein keratin is inserted. They eventually reach the corneum and slough off (desquamation). This process is called "keratinization". This keratinized layer of skin is responsible for keeping water in the body and keeping other harmful chemicals and pathogensout, making skin a natural barrier to infection.
Components
The epidermis contains no blood vessels, and is nourished by diffusion from the dermis. The main type of cells which make up the epidermis are keratinocytes,melanocytes, Langerhans cells and Merkels cells. The epidermis helps the skin to regulate body temperature.[citation needed]
Layers
Epidermis is divided into several layers where cells are formed through mitosis at the innermost layers. They move up the strata changing shape and composition as they differentiate and become filled with keratin. They eventually reach the top layer calledstratum corneum and are sloughed off, or desquamated. This process is calledkeratinization and takes place within weeks. The outermost layer of the epidermis consists of 25 to 30 layers of dead cells.
Sublayers
Epidermis is divided into the following 5 sublayers or strata:
- Stratum corneum
- Stratum lucidum
- Stratum granulosum
- Stratum spinosum
- Stratum germinativum (also called "stratum basale").
Blood capillaries are found beneath the epidermis, and are linked to an arteriole and a venule. Arterial shunt vessels may bypass the network in ears, the nose and fingertips.
| Dermis | |
|---|---|

The distribution of the bloodvessels in the skin of the sole of the foot. (Corium - TA alternate term for dermis - is labeled at upper right.)
| |

A diagrammatic sectional view of the skin (click on image to magnify). (Dermis labeled at center right.)
| |
| Identifiers | |
| Gray's | p.1065 |
| MeSH | A17.815.180 |
| Dorlands /Elsevier | Skin |
| Anatomical terminology | |
Dermis
Main article: Dermis
The dermis is the layer of skin beneath the epidermis that consists ofconnective tissue and cushions the body from stress and strain. The dermis is tightly connected to the epidermis by a basement membrane. It also harbors many nerve endings that provide the sense of touch and heat. It contains thehair follicles, sweat glands, sebaceous glands, apocrine glands, lymphatic vessels and blood vessels. The blood vessels in the dermis provide nourishment and waste removal from its own cells as well as from the Stratum basale of the epidermis.
The dermis is structurally divided into two areas: a superficial area adjacent to the epidermis, called the papillary region, and a deep thicker area known as the reticular region.
Papillary region
The papillary region is composed of loose areolar connective tissue. It is named for its fingerlike projections called papillae, that extend toward the epidermis. The papillae provide the dermis with a "bumpy" surface that interdigitates with the epidermis, strengthening the connection between the two layers of skin.
In the palms, fingers, soles, and toes, the influence of the papillae projecting into the epidermis forms contours in the skin's surface. These epidermal ridges occur in patterns (see: fingerprint) that are genetically and epigenetically determined and are therefore unique to the individual, making it possible to use fingerprints or footprints as a means of identification.
Reticular region
The reticular region lies deep in the papillary region and is usually much thicker. It is composed of dense irregular connective tissue, and receives its name from the dense concentration of collagenous, elastic, and reticular fibers that weave throughout it. These protein fibers give the dermis its properties of strength, extensibility, and elasticity.
Also located within the reticular region are the roots of the hair, sebaceous glands, sweat glands, receptors, nails, and blood vessels.
Tattoo ink is held in the dermis. Stretch marks from pregnancy are also located in the dermis.
Hypodermis
The hypodermis is not part of the skin, and lies below the dermis. Its purpose is to attach the skin to underlying bone andmuscle as well as supplying it with blood vessels and nerves. It consists of loose connective tissue and elastin. The main cell types are fibroblasts, macrophages and adipocytes (the hypodermis contains 50% of body fat). Fat serves as padding and insulation for the body.
Permeability
Human skin has a low permeability; that is, most foreign substances are unable to penetrate and diffuse through the skin. Skin's outermost layer, the stratum corneum, is an effective barrier to most inorganic nanosized particles.[22][23] This protects the body from external particles such as toxins by not allowing them to come into contact with internal tissues. However in some cases it is desirable to allow particles entry to the body through the skin. Potential medical applications of such particle transfer has prompted developments in nanomedicine and biology to increase skin permeability. One application of transcutaneous particle delivery could be to locate and treat cancer. Nanomedical researchers seek to target the epidermis and other layers of active cell division where nanoparticles can interact directly with cells that have lost their growth-control mechanisms (cancer cells). Such direct interaction could be used to more accurately diagnose properties of specific tumors or to treat them by delivering drugs with cellular specificity.
Nanoparticles
Nanoparticles 40 nm in diameter and smaller have been successful in penetrating the skin.[24][25][26] Research confirms that nanoparticles larger than 40 nm do not penetrate the skin past the stratum corneum.[24] Most particles that do penetrate will diffuse through skin cells, but some will travel down hair follicles and reach the dermis layer.
The permeability of skin relative to different shapes of nanoparticles has also been studied. Research has shown that spherical particles have a better ability to penetrate the skin compared to oblong (ellipsoidal) particles because spheres are symmetric in all three spatial dimensions.[26] One study compared the two shapes and recorded data that showed spherical particles located deep in the epidermis and dermis whereas ellipsoidal particles were mainly found in the stratum corneum and epidermal layers.[27] Nanorods are used in experiments because of their unique fluorescent properties but have shown mediocre penetration.
Nanoparticles of different materials have shown skin’s permeability limitations. In many experiments, gold nanoparticles 40 nm in diameter or smaller are used and have shown to penetrate to the epidermis. Titanium oxide (TiO2), zinc oxide(ZnO), and silver nanoparticles are ineffective in penetrating the skin past the stratum corneum.[28][29] Cadmium selenide(CdSe) quantum dots have proven to penetrate very effectively when they have certain properties. Because CdSe is toxic to living organisms, the particle must be covered in a surface group. An experiment comparing the permeability of quantum dots coated in polyethylene glycol (PEG), PEG-amine, and carboxylic acid concluded the PEG and PEG-amine surface groups allowed for the greatest penetration of particles. The carboxylic acid coated particles did not penetrate past the stratum corneum.[27]
Increasing permeability
Scientists previously believed that the skin was an effective barrier to inorganic particles. Damage from mechanical stressors was believed to be the only way to increase its permeability.[30] Recently, however, simpler and more effective methods for increasing skin permeabiltiy have been developed. For example, ultraviolet radiation (UVR) has been used to slightly damage the surface of skin, causing a time-dependent defect allowing easier penetration of nanoparticles.[31] The UVR’s high energy causes a restructuring of cells, weakening the boundary between the stratum corneum and the epidermal layer.[32][31] The damage of the skin is typically measured by the transepidermal water loss (TEWL), though it may take 3–5 days for the TEWL to reach its peak value. When the TEWL reaches its highest value, the maximum density of nanoparticles is able to permeate the skin. Studies confirm that UVR damaged skin significantly increases the permeability.[32][31] The effects of increased permeability after UVR exposure can lead to an increase in the number of particles that permeate the skin. However, the specific permeability of skin after UVR exposure relative to particles of different sizes and materials has not been determined.[31]
Other skin damaging methods used to increase nanoparticle penetration include tape stripping, skin abrasion, and chemical enhancement. Tape stripping is the process in which tape is applied to skin then lifted to remove the top layer of skin. Skin abrasion is done by shaving the top 5-10 micrometers off the surface of the skin. Chemical enhancement is the process in which chemicals such as polyvinylpyrrolidone (PVP), dimethyl sulfoxide (DMSO), and oleic acid are applied to the surface of the skin to increase permeability.[33][34]
Electroporation is the application of short pulses of electric fields on skin and has proven to increase skin permeability. The pulses are high voltage and on the order of milliseconds when applied. Charged molecules penetrate the skin more frequently than neutral molecules after the skin has been exposed to electric field pulses. Results have shown molecules on the order of 100 micrometers to easily permeate electroporated skin.[34]
Applications
A large area of interest in nanomedicine is the transdermal patch because of the possibility of a painless application of therapeutic agents with very few side effects. Transdermal patches have been limited to administer a small number of drugs, such as nicotine, because of the limitations in permeability of the skin. Development of techniques that increase skin permeability has led to more drugs that can be applied via transdermal patches and more options for patients.[34]
Increasing the permeability of skin allows nanoparticles to penetrate and target cancer cells. Nanoparticles along with multi-modal imaging techniques have been used as a way to diagnose cancer non-invasively. Skin with high permeability allowed quantum dots with an antibody attached to the surface for active targeting to successfully penetrate and identify canceroustumors in mice. Tumor targeting is beneficial because the particles can be excited using fluorescence microscopy and emit light energy and heat that will destroy cancer cells.[35]
Sunblock and sunscreen
Although some believe that sunblock and sunscreen are both the same, they are not, although they have similar properties and are both important in caring of the skin.[36]
Sunblock Sunblock is opaque and is stronger than sunscreen since it is able to block majority of the UVA/UVB rays and radiation from the sun, thus not having to be reapplied several times a day. Titanium dioxide and zinc oxide are two of the important ingredients in sunblock.
Sunscreen Sunscreen is more transparent once applied to the skin and also has the ability to protect against UVA/UVB rays as well, although the sunscreen's ingredients have the ability to break down at a faster rate once exposed to sunlight, and some of the radiation is able to penetrate to the skin. In order for sunscreen to be more effective it is necessary to consistently reapply and use a higher spf.
Nutrition for healthy skin
Vitamin A, also known as retinoids, benefits the skin by normalizing keratinization, downregulating sebum production which contributes to acne, and reversing and treating photodamage, striae, and cellulite.
Vitamin D and analogs are used to downregulate the cutaneous immune system and epithelial proliferation while promoting differentiation.
Vitamin C is an antioxidant that regulates collagen synthesis, forms barrier lipids, regenerates vitamin E, and provides photoprotection.
Vitamin E is a membrane antioxidant that protects against oxidative damage and also provides protection against harmful UVrays. [37]
Several scientific studies confirmed that changes in baseline nutritional status affects skin condition. [38]
Skin overview
Nail (anatomy)
For the nail on a bird's beak, see Beak#Nail.
"Toenail" redirects here. For the construction technique, see Toenailing.
| Nail | |
|---|---|
 | |

A gorilla's fingernails
| |
| Details | |
| Latin | unguis |
| Identifiers | |
| Anatomical terminology | |
A nail is a horn-like envelope covering the tips of the fingers and toes in humans, most non-human primates, and a few other mammals. Nails are similar to claws in other animals. Fingernails and toenails are made of a tough protective protein called keratin. This protein is also found in the hooves and horns of different animals. The mammalian nail, claw, and hoof are all examples of ungues [singular unguis].
Contents
Structure[edit]
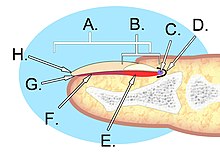
The nail consists of the nail plate, the nail matrix and the nail bed below it, and the grooves surrounding it.[1]
Parts of the nail
The matrix, sometimes called[2] the matrix unguis, keratogenous membrane, nail matrix, or onychostroma, is thetissue (or germinal matrix) which the nail protects.[3] It is the part of the nail bed that is beneath the nail and contains nerves, lymphand blood vessels.[4] The matrix is responsible for producing cells that become the nail plate. The width and thickness of the nail plate is determined by the size, length, and thickness of the matrix, while the shape of the fingertip itself shows if the nail plate is flat, arched or hooked.[5] The matrix will continue to grow as long as it receives nutrition and remains in a healthy condition.[4] As new nail plate cells are made, they push older nail plate cells forward; and in this way older cells become compressed, flat, and translucent. This makes the capillaries in the nail bed below visible, resulting in a pink color.[6]
The lunula ("small moon") is the visible part of the matrix, the whitish crescent-shaped base of the visible nail.[7] The lunula can best be seen in the thumb and may not be visible in the little finger.
The nail bed is the skin beneath the nail plate.[7] Like all skin, it is made of two types of tissues: the deeper dermis, the living tissue which includes capillaries and glands,[8] and the epidermis, the layer just beneath the nail plate, which moves toward the finger tip with the plate. The epidermis is attached to the dermis by tiny longitudinal "grooves"[5] called matrix crests (cristae matricis unguis).[3][8] In old age, the nail plate becomes thinner and these grooves become more visible.[5]
The nail sinus (sinus unguis) is where the nail root is;[3] i.e. the base of the nail underneath the skin. It originates from the actively growing tissue below, the matrix.[4]
The nail plate (corpus unguis)[3] is the hard part of the nail, made of translucent keratin protein. Several layers of dead, compacted cells cause the nail to be strong but flexible.[5] Its (transverse) shape is determined by the form of the underlying bone.[5] In common usage, the word nail often refers to this part only.
The free margin (margo liber) or distal edge is the anterior margin of the nail plate corresponding to the abrasive or cutting edge of the nail.[3] The hyponychium (informally known as the "quick")[9] is the epithelium located beneath the nail plate at the junction between the free edge and the skin of the fingertip. It forms a seal that protects the nail bed.[4] Theonychodermal band is the seal between the nail plate and the hyponychium. It is just under the free edge, in that portion of the nail where the nail bed ends and can be recognized in fair-skinned people by its glassy, greyish colour. It is not visible in some individuals while it is highly prominent on others.[5]
Together, the eponychium and the cuticle form a protective seal. The cuticle is the semi-circular layer of non-living, almost invisible dead skin cells that "ride out on" and cover the back of the visible nail plate while the Eponychium is the fold of skin cells that produces the cuticle. It is the cuticle that is removed during a manicure, but the Eponychium should not be touched due to risk of infection.[6] The eponychium is a small band of living cells (epithelium) that extends from the posterior nail wall onto the base of the nail.[3] The eponychium is the end of the proximal fold that folds back upon itself to shed an epidermal layer of skin onto the newly formed nail plate.[contradictory]. The perionyx is the projecting edge of the eponychium covering the proximal strip of the lunula.[3]
The nail wall (vallum unguis) is the cutaneous fold overlapping the sides and proximal end of the nail. The lateral margin(margo lateralis) lies beneath the nail wall on the sides of the nail and the nail groove or fold (sulcus matricis unguis) are the cutaneous slits into which the lateral margins are embedded.[3]
The paronychium is the border tissue around the nail[10] and paronychia is an infection in this area.
Function
A healthy fingernail has the function of protecting the distal phalanx, the fingertip, and the surrounding soft tissues from injuries. It also serves to enhance precise delicate movements of the distal digits through counter-pressure exerted on the pulp of the finger. [1] The nail then acts as a counterforce when the end of the finger touches an object, thereby enhancing the sensitivity of the fingertip,[11] even though there are no nerve endings in the nail itself. Finally, the nail functions as a tool, enabling for instance a so-called "extended precision grip" (e.g. pulling out a splinter in one's finger), and certain cutting or scraping actions.
Growth
The growing part of the nail is under the skin at the nail's proximal end under the epidermis, which is the only living part of a nail.
In mammals, the growth rate of nails is related to the length of the terminal phalanges (outermost finger bones). Thus, in humans, the nail of the index finger grows faster than that of the little finger; and fingernails grow up to four times faster than toenails. [12]
In humans, nails grow at an average rate of 3 mm (0.12 in) a month.[13] Fingernails require three to six months to regrow completely, and toenails require 12 to 18 months. Actual growth rate is dependent upon age, sex, season, exercise level, diet, and hereditary factors.[14] Contrary to popular belief, nails do not continue to grow after death; the skin dehydrates and tightens, making the nails (and hair) appear to grow.[15]
Permeability
The nail is often considered an impermeable barrier, but this is not true. In fact, it is much more permeable than the skin,[16]and the composition of the nail includes 7–12% water. This permeability has implications for penetration by harmful and medicinal substances; in particular cosmetics applied to the nails can pose a risk. Water can penetrate the nail as can many other substances including paraquat, a fast acting herbicide that is harmful to humans, urea which is often an ingredient in creams and lotions meant for use on hands and fingers, and several fungicidal agents such as salicylic acid, miconazolebranded Monistat, natamycin; and sodium hypochlorite which is the active ingredient in common household bleach (but usually only in 2–3% concentration).[16]
Clinical significance
Healthcare and pre-hospital-care providers (EMTs or paramedics) often use the fingernail beds as a cursory indicator of distal tissue perfusion of individuals who may be dehydrated or in shock.[17] However, this test is not considered reliable in adults.[18] This is known as the CRT or blanch test. The fingernail bed is briefly depressed to turn the nailbed white. When the pressure is released, the normal pink colour should be restored within a second or two. Delayed return to pink colour can be an indicator of certain shock states such as hypovolemia.[19][20]
Nail growth record can show the history of recent health and physiological imbalances, and has been used as a diagnostic tool since ancient times.[21] Deep transverse grooves known as Beau's lines may form across the nails (not along the nail from cuticle to tip) and are usually a natural consequence of aging, though they may result from disease. Discoloration, thinning, thickening, brittleness, splitting, grooves, Mees' lines, small white spots, receded lunula, clubbing (convex), flatness, spooning (concave) can indicate illness in other areas of the body, nutrientdeficiencies, drug reaction or poisoning, or merely local injury. Nails can also become thickened (onychogryphosis), loosened (onycholysis), infected with fungus (onychomycosis) or degenerate (onychodystrophy); for further information seenail diseases.
DNA profiling is a technique employed by forensic scientists on hair, fingernails etc.
Health and care
The best way to care for nails is to trim them regularly. Bluish or purple fingernail beds may be a symptom of peripheral cyanosis, which indicates oxygen deprivation.
Nails can dry out, just like skin. They can also peel, break, and be infected. Toe infections, for instance, can be caused or exacerbated by dirty socks, specific types of aggressiveexercise,[which?] tight footwear, and walking unprotected in an uncleanenvironment.[citation needed] Common organisms causing nail infections include yeasts andmoulds (particularly dermatophytes).[22]
Nail tools used by different people may transmit infections. To avoid this, new improved contactless tools can be used, for example, gel and cream cuticle removers instead of cuticle scissors.
Nail disease can be very subtle and should be evaluated by a dermatologist with a focus in this particular area of medicine.[23] However, most times it is a nail technician who will note a subtle change in nail disease.
Inherited accessory nail of the fifth toe occurs where the toenail of the smallest toe is separated, forming a smaller, "sixth toenail" in the outer corner of the nail.[citation needed]Like any other nail, it can be cut using a nail clipper.
Effect of nutrition
Vitamin A is an essential micronutrient for vision, reproduction, cell and tissue differentiation, and immune function. Vitamin D and calcium work together in cases of maintaining homeostasis, creating muscle contraction, transmission of nerve pulses, blood clotting, and membrane structure. A lack of vitamin A, vitamin D, or calcium can cause dryness and brittleness.
Insufficient vitamin B12 can lead to excessive dryness, darkened nails, and rounded or curved nail ends. Insufficient intake of both vitamin A and B results in fragile nails with horizontal and vertical ridges. Some over-the-counter vitamin supplements such as certain multivitamins and biotin may help in growth of strong nails, although this is quite subjective.[24]
Protein is a building material for new nails; therefore, low dietary protein intake may cause anemia and the resultant reduced hemoglobin in the blood filling the capillaries of the nail bed reflects varying amounts of light incident on the nail matrix resulting in lighter shades of pink ultimately resulting in white nail beds when the hemoglobin is very low. When hemoglobin is close to 15 or 16 grams, most of the spectrum of light is absorbed and only the pink color is reflected back and the nails look pink. A lack of protein combined with deficiencies in folic acid and vitamin C produce hangnails.
Essential fatty acids play a large role in healthy skin as well as nails. Splitting and flaking of nails may be due to a lack oflinoleic acid.
Iron-deficiency anemia can lead to a pale color along with a thin, brittle, ridged texture. Iron deficiency in general may cause the nails to become flat or concave, rather than convex. Heme iron is absorbed fairly easily in comparison to non-heme iron; however, both types provide the necessary bodily functions.[25]
Society and culture
Many people also compulsively bite their nails.
Fashion
Manicures (for the hands) and pedicures (for the feet) are health and cosmetic procedures to groom, trim, and paint the nails and manage calluses. They require various tools such as cuticle scissors, nail scissors, nail clippers, andnail files. Artificial nails can also be fixed onto real nails for cosmetic purposes.
A person whose occupation is to cut, shape and care for nails as well as to apply overlays such as acrylic and UV gel is sometimes called a nail technician. The place where a nail technician works may be a nail salon or nail shop or nail bar.
Painting the nails with coloured nail polish (also called nail lacquer and nail varnish) to improve the appearance is a common practice dating back to at least 3000 B.C.
Length records[edit]
Guinness World Records began tracking record fingernail lengths in 1955, when a Chinese priest was listed as having fingernails 1 foot 10.75 inches (57.79 cm) long.
The current record-holder for men, according to Guinness, is Shridhar Chillal from India who set the record in 1998 with a total of 20 feet 2.25 inches (615.32 cm) of nails on his left hand. His longest nail, on his thumb, was 4 feet 9.6 inches (146.3 cm) long.
The record-holder for women is Lee Redmond of the U.S., who set the record in 2001 and as of 2008 had nails with a total length on both hands of 28 feet (850 cm), with the longest nail on her right thumb at 2 feet 11 inches (89 cm).[26]
In other animals[edit]
The nails of primates and the hooves of running mammals evolved from the claws of earlier animals.[27]
In contrast to nails, claws are typically curved ventrally (downwards in animals) and compressed sideways. They serve a multitude of functions —including climbing, digging, and fighting— and have undergone numerous adaptive changes in different animal taxa. Claws are pointed at their ends and are composed of two layers: a thick, deep layer and a superficial, hardened layer which serves a protective function. The underlying bone is a virtual mould of the overlying horny structure and therefore has the same shape as the claw or nail. Compared to claws, nails are flat, less curved, and do not extend far beyond the tip of the digits. The ends of the nails usually consist only of the "superficial", hardened layer and are not pointed like claws.[27]
With only a few exceptions, primates retain plesiomorphic (original, "primitive") hands with five digits, each equipped with either a nail or a claw. For example, nearly all livingstrepsirrhine primates have nails on all digits except the second toe which is equipped with agrooming claw. Tarsiers have a grooming claw on second and third toes. Less commonly known, a grooming claw is also found on the second pedal digit of owl monkeys (Aotus), titis (Callicebus), and possibly otherNew World monkeys.[28] The needle-clawed bushbaby (Euoticus) has keeled nails (the thumb and the first and the second toes have claws) featuring a central ridge that ends in a needle-like tip. In tree shrews all digits have claws and, unlike most primates, the digits of their feet are positioned close together, and therefore the thumb cannot be brought into opposition (another distinguishing feature of primates).[27]
A study of the fingertip morphology of four small-bodied New World monkey species indicated a correlation between increasing small-branch foraging and
- expanded apical pads (fingertips),
- developed epidermal ridges (fingerprints),
- broadened distal parts of distal phalanges (fingertip bones), and
- reduced flexor and extensor tubercles (attachments areas for finger muscles on bones).
This suggests that whereas claws are useful on large-diameter branches, wide fingertips with nails and epidermal ridges were required for habitual locomotion on small-diameter branches. It also indicates keel-shaped nails of Callitrichines (a family of New World monkeys) is a derived postural adaptation rather than retained ancestral condition. [29]










No comments:
Post a Comment