- iiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiiii
Skeletal system Bones supporting the body and its organs.
- Our skeleton consists of all our bones, teeth, cartilage, and joints. Some bones protect our internal organs. Some bones provide a framework for the body (just as the spokes of an umbrella provide a framework). Some bones contain red marrow that produces blood cells and yellow marrow that also stores fat.
- "Bone structure" and "skeletal system" redirect here. For skeletal systems of other animals, see Skeleton.
Human skeleton  Diagram of the human skeleton
Diagram of the human skeletonDetails Greek σκελετός Anatomical terminology The human skeleton is the internal framework of the body. It is composed of 270 bones at birth – this total decreases to 206 bones by adulthood after some bones have fused together.[1] The bone mass in the skeleton reaches maximum density around age 30. The human skeleton can be divided into theaxial skeleton and the appendicular skeleton. The axial skeleton is formed by the vertebral column, the rib cage and the skull. The appendicular skeleton, which is attached to the axial skeleton, is formed by the pectoral girdle, thepelvic girdle and the bones of the upper and lower limbs.The human skeleton serves six major functions; support, movement, protection, production of blood cells, storage of ions and endocrine regulation.The human skeleton is not as sexually dimorphic as that of many other primate species, but subtle differences between sexes in the morphology of the skull,dentition, long bones, and pelves exist. In general, female skeletal elements tend to be smaller and less robust than corresponding male elements within a given population. The human female pelvis is also different from that of males in order to facilitate child birth.[citation needed] Unlike most primates, human males do not have penile bones.[2]Contents
[hide]Divisions
Axial skeleton
Main article: Axial skeletonThe axial skeleton (80 bones) is formed by the vertebral column (32–34 bones; the number of the vertebrae differs from human to human as the lower 2 parts, sacral and coccygeal bone may vary in length), the rib cage (12 pairs of ribs and thesternum), and the skull (22 bones and 7 associated bones).The upright posture of humans is maintained by the axial skeleton, which transmits the weight from the head, the trunk, and the upper extremities down to the lower extremities at the hip joints. The bones of the spine are supported by many ligaments. The erector spinae muscles are also supporting and are useful for balance.A human is able to survive with just the axial portion of their skeleton.Appendicular skeleton
Main article: Appendicular skeletonThe appendicular skeleton (126 bones) is formed by the pectoral girdles, the upper limbs, the pelvic girdle or pelvis, and the lower limbs. Their functions are to make locomotion possible and to protect the major organs of digestion, excretion and reproduction.Functions
The skeleton serves six major functions; support, movement, protection, production of blood cells, storage of minerals and endocrine regulation.Support
The skeleton provides the framework which supports the body and maintains its shape. The pelvis, associated ligaments and muscles provide a floor for the pelvic structures. Without the rib cages, costal cartilages, and intercostal muscles, thelungs would collapse.Movement
The joints between bones allow movement, some allowing a wider range of movement than others, e.g. the ball and socket joint allows a greater range of movement than the pivot joint at the neck. Movement is powered by skeletal muscles, which are attached to the skeleton at various sites on bones. Muscles, bones, and joints provide the principal mechanics for movement, all coordinated by the nervous system.It is believed that the reduction of human bone density in prehistoric times reduced the agility and dexterity of human movement. Shifting from hunting to agriculturehave caused human bone density to reduce significantly.[3][4][5]Protection
The skeleton helps protect our many vital internal organs from being damaged.- The skull protects the brain, the eyes, and the middle and inner ears.
- The vertebrae protect the spinal cord.
- The rib cage, spine, and sternum protect the lungs, heart and major blood vessels.
- The clavicle and scapula protect the shoulder.
- The ilium and spine protect the digestive and urogenital systems and the hip.
- The patella and the ulna protect the knee and the elbow respectively.
- The carpals and tarsals protect the wrist and ankle respectively.
Blood cell production
The skeleton is the site of haematopoiesis, the development of blood cells that takes place in the bone marrow. In children, haematopoiesis occurs primarily in the marrow of the long bones such as the femur and tibia. In adults, it occurs mainly in the pelvis, cranium, vertebrae, and sternum.[6]Storage
The bone matrix can store calcium and is involved in calcium metabolism, and bone marrow can store iron in ferritin and is involved in iron metabolism. However, bones are not entirely made of calcium, but a mixture of chondroitin sulfate andhydroxyapatite, the latter making up 70% of a bone. Hydroxyapatite is in turn composed of 39.8% of calcium, 41.4% of oxygen, 18.5% of phosphorus, and 0.2% of hydrogen by mass. Chondroitin sulfate is a sugar made up primarily of oxygen and carbon.Endocrine regulation
Bone cells release a hormone called osteocalcin, which contributes to the regulation of blood sugar (glucose) and fat deposition. Osteocalcin increases both the insulin secretion and sensitivity, in addition to boosting the number of insulin-producing cells and reducing stores of fat.[7]Sex differences
Anatomical differences between human males and females are highly pronounced in some soft tissue areas, but tend to be limited in the skeleton. The human skeleton is not as sexually dimorphic as that of many other primate species, but subtle differences between sexes in the morphology of the skull, dentition, long bones, and pelves (sing. pelvis) are exhibited across human populations. In general, female skeletal elements tend to be smaller and less robust than corresponding male elements within a given population.Skull
A variety of gross morphological traits of the human skull demonstrate sexual dimorphism, such as the nuchal crest, mastoid processes, supraorbital margin, supraorbital ridge, and mental eminence.[8]Dentition
Human inter-sex dental dimorphism centers on the canines, but it is not nearly as pronounced as in the other great apes.Long bones
Long bones are generally larger in males than in females within a given population. Muscle attachment sites on long bones are often more robust in males than in females, reflecting a difference in overall muscle mass and development between sexes. Sexual dimorphism in the long bones is commonly characterized by morphometric or gross morphological analyses.Pelvis
Human pelves exhibit greater sexual dimorphism than other bones, specifically in the size and shape of the pelvic cavity, ilia, greater sciatic notches, and the sub-pubic angle. The Phenice method is commonly used to determine the sex of an unidentified human skeleton by anthropologists with 96% to 100% accuracy in some populations.[9]Disorders
See also: Bone diseaseThere are many classified skeletal disorders. One of the most common is osteoporosis. Also common is scoliosis, a side-to-side curve in the back or spine, often creating a pronounced "C" or "S" shape when viewed on an x-ray of the spine. This condition is most apparent during adolescence, and is most common with females.Arthritis[edit]
Main article: ArthritisArthritis is a disorder of the joints. It involves inflammation of one or more joints. When affected by arthritis, the joint or joints affected may be painful to move, may move in unusual directions or may be immobile completely. The symptoms of arthritis will vary differently between types of arthritis. The most common form of arthritis: Osteoarthritis can affect both the larger and smaller joints of the human skeleton. The cartilage in the affected joints will degrade, soften and wear away. This decreases the mobility of the joints and decreases the space between bones where cartilage should be.Osteoporosis
Main article: OsteoporosisOsteoporosis is a disease of bone where there is reduced bone mineral density, increasing the likelihood of fractures.[10]Osteoporosis is defined by the World Health Organization in women as a bone mineral density 2.5 standard deviations below peak bone mass, relative to the age and sex-matched average, as measured by Dual energy X-ray absorptiometry, with the term "established osteoporosis" including the presence of a fragility fracture.[11] Osteoporosis is most common in women after menopause, when it is called "postmenopausal osteoporosis", but may develop in men and premenopausal women in the presence of particular hormonal disorders and other chronic diseases or as a result of smoking and medications, specifically glucocorticoids.[10] Osteoporosis usually has no symptoms until a fracture occurs.[10] For this reason, DEXA scans are often done in people with one or more risk factors, who have developed osteoporosis and be at risk of fracture.[10]Osteoporosis treatment includes advice to stop smoking, decrease alcohol consumption, exercise regularly, and have a healthy diet. Calcium supplements may also be advised, as may Vitamin D. When medication is used, it may includebisphosphonates, Strontium ranelate, and osteoporosis may be one factor considered when commencing Hormone replacement therapy.[10] Bone
From Wikipedia, the free encyclopediaThis article is about the skeletal organ. For other uses, see Bone (disambiguation) and Bones (disambiguation).Bone  A bone dating from the Pleistocene Ice Age of an extinct species of elephant.
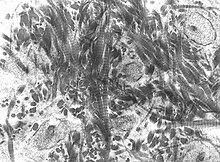
A bone dating from the Pleistocene Ice Age of an extinct species of elephant. A scanning electronic micrograph of bone at 10,000x magnification.
A scanning electronic micrograph of bone at 10,000x magnification.Anatomical terminology A bone is a rigid organ that constitutes part of the vertebral skeleton. Bones support and protect the various organs of the body, produce red and white blood cells, store minerals and also enable mobility. Bone tissue is a type of dense connective tissue. Bones come in a variety of shapes and sizes and have a complex internal and external structure. They are lightweight yet strong and hard, and serve multiple functions. Mineralized osseous tissue or bone tissue, is of two types – cortical and cancellous and gives it rigidity and a coral-like three-dimensional internal structure. Other types of tissue found in bones include marrow, endosteum, periosteum, nerves, blood vessels and cartilage.Bone is an active tissue composed of different cells. Osteoblasts are involved in the creation and mineralisation of bone; osteocytes and osteoclasts are involved in the reabsorption of bone tissue. The mineralised matrix of bone tissue has an organic component mainly of collagen and an inorganic component of bone mineral made up of various salts.In the human body at birth, there are over 270 bones,[1] but many of these fuse together during development, leaving a total of 206 separate bones in the adult,[2] not counting numerous small sesamoid bones. The largest bone in the body is the thigh-bone (femur) and the smallest is the stapes in the middle ear.Structure
Main article: Osseous tissueBone is not a uniformly solid material, but is mostly a matrix. The primary tissue of bone, osseous tissue, is relatively hard and lightweight. Its matrix is mostly made up of a composite material incorporating the inorganic mineralcalcium phosphate in the chemical arrangement termed calciumhydroxylapatite (this is the osseous tissue that gives bones their rigidity) and organic collagen, an elastic protein which improves fracture resistance.[3]Bone is formed by the hardening of this matrix around entrapped cells. When these cells become entrapped from osteoblasts they become osteocytes.[citation needed]Layered structure
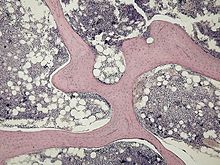
Cortical bone
The hard outer layer of bones is composed of cortical bone also called compact bone. Cortical referring to the outer (cortex) layer. The hard outer layer gives bone its smooth, white, and solid appearance, and accounts for 80% of the total bone mass of an adult skeleton.[citation needed]Cortical bone consists of multiple microscopic columns, each called an osteon. Each column is multiple layers of osteoblasts and osteocytes around a central canal called the Haversian canal. Volkmann's canals at right angles connect the osteons together. The columns are metabolically active, and as bone is reabsorbed and created the nature and location of the cells within the osteon will change. Cortical bone is covered by a periosteum on its outer surface, and an endosteum on its inner surface. The endosteum is the boundary between the cortical bone and the cancellous bone. [4]Cancellous bone
Filling the interior of the bone is the cancellous bone also known as trabecular or spongy bone tissue.[4] It is an open cell porous network. Thin formations ofosteoblasts covered in endosteum create an irregular network of spaces.[5] Within these spaces are bone marrow and hematopoietic stem cells that give rise toplatelets, red blood cells and white blood cells.[5] Trabecular marrow is composed of a network of rod- and plate-like elements that make the overall organ lighter and allow room for blood vessels and marrow. Trabecular bone accounts for the remaining 20% of total bone mass but has nearly ten times the surface area of compact bone.[6]Bone marrow
Bone marrow, also known as myeloid tissue, can be found in almost any bone that holds cancellous tissue. In newborns, all such bones are filled exclusively with red marrow, but as the child ages it is mostly replaced by yellow, or fatty marrow. In adults, red marrow is mostly found in the bone marrow of the femur, the ribs, the vertebrae and pelvic bones.[citation needed]Composition
Main article: Osseous tissueCells
Bone is a metabolically active tissue composed of several types of cells. These cells include osteoblasts, which are involved in the creation and mineralization of bone tissue, osteocytes, and osteoclasts, which are involved in the reabsorption of bone tissue. Osteoblasts and osteocytes are derived from osteoprogenitor cells, butosteoclasts are derived from the same cells that differentiate to form macrophagesand monocytes.[7] Within the marrow of the bone there are also hematopoietic stem cells. These cells give rise to other cells, including white blood cells, red blood cells, and platelets.[8]- Osteoblasts are mononucleate bone-forming cells. They are located on the surface of osteoid seams and make a protein mixture known as osteoid, which mineralizes to become bone.[9] The osteoid seam is a narrow region of newly formed organic matrix, not yet mineralized, located on the surface of a bone. Osteoid is primarily composed of Type I collagen. Osteoblasts also manufacture hormones, such as prostaglandins, to act on the bone itself. They robustly produce alkaline phosphatase, an enzyme that has a role in the mineralisation of bone, as well as many matrix proteins.
- Osteocytes are mostly inactive osteoblasts.[7] Osteocytes originate from osteoblasts that have migrated into and become trapped and surrounded by bone matrix that they themselves produced.[4] The spaces they occupy are known as lacunae. Osteocytes have many processes that reach out to meet osteoblasts and other osteocytes probably for the purposes of communication.[citation needed]
- Osteoclasts are the cells responsible for bone resorption, thus they break down bone. New bone is then formed by the osteoblasts. Bone is constantlyremodelled by the resorption of osteoclasts and created by osteoblasts.[7]Osteoclasts are large cells with multiple nuclei located on bone surfaces in what are called Howship's lacunae (or resorption pits). These lacunae are the result of surrounding bone tissue that has been reabsorbed.[10] Because the osteoclasts are derived from a monocyte stem-cell lineage, they are equipped withphagocytic-like mechanisms similar to circulating macrophages.[7] Osteoclasts mature and/or migrate to discrete bone surfaces. Upon arrival, active enzymes, such as tartrate resistant acid phosphatase, are secreted against the mineral substrate.[citation needed] The reabsorption of bone by osteoclasts also plays a role in calcium homeostasis.[10]
Extracellular[edit]
Bones consist of living cells embedded in a mineralized organic matrix. This matrix consists of organic components, mainlycollagen - "organic" referring to materials produced as a result of the human body - and inorganic components, primarilyhydroxyapatite and other salts of calcium and phosphate. Above 30% of the acellular part of bone consists of the organic components, and 70% of salts.[11] The strands of collagen give bone its tensile strength, and the interspersed crystals ofhydroxyapatite give bone its compressional strength. These effects are synergistic.[11]The inorganic composition of bone (bone mineral) is primarily formed from salts ofcalcium and phosphate, the major salt being hydroxyapatite (Ca10(PO4)6(OH)2).[11]The exact composition of the matrix may change over time and with nutrition, with the ratio of calcium to phosphate varying between 1.3-2 (per weight), and trace minerals such as magnesium, sodium, potassium and carbonate also being found.[11]The organic part of matrix is mainly composed of Type I collagen.[11][12] Collagen composes about 90-95% of the organic matrix, with remainder of the matrix being a homogenous liquid called ground substance consisting of proteoglycans such ashyaluronic acid and chondroitin sulfate.[11] Collagen consists of strands of repeating units, which give bone tensile strength, and are arranged in an overlapping fashion that prevents sheer stress. The function of ground substance is not fully known.[11]Two types of bone can be identified microscopically according to the arrangement of collagen:- Woven bone, which is characterized by haphazard organization of collagen fibers and is mechanically weak[13]
- Lamellar bone, which has a regular parallel alignment of collagen into sheets ("lamellae") and is mechanically strong [13]
Woven bone is produced when osteoblasts produce osteoid rapidly, which occurs initially in all fetal bones, but is later replaced by more resilient lamellar bone. In adults woven bone is created after fractures or in Paget's disease. Woven bone is weaker, with a smaller number of randomly oriented collagen fibers, but forms quickly; it is for this appearance of the fibrous matrix that the bone is termed woven. It is soon replaced by lamellar bone, which is highly organized in concentric sheets with a much lower proportion of osteocytes to surrounding tissue. Lamellar bone, which makes its first appearance in the fetus during the third trimester,[14] is stronger and filled with many collagen fibers parallel to other fibers in the same layer (these parallel columns are called osteons). In cross-section, the fibers run in opposite directions in alternating layers, much like in plywood, assisting in the bone's ability to resist torsion forces. After a fracture, woven bone forms initially and is gradually replaced by lamellar bone during a process known as "bony substitution." Compared to woven bone, lamellar bone formation takes place more slowly. The orderly deposition of collagen fibers restricts the formation of osteoid to about 1 to 2 µm per day. Lamellar bone also requires a relatively flat surface to lay the collagen fibers in parallel or concentric layers.[citation needed]- Deposition
The extracellular matrix of bone is laid down by osteoblasts, which secrete both collagen and ground substance. These synthesise collagen within the cell, and then secrete collagen fibrils. The collagen fibres rapidly polymerise to form collagen strands. At this stage they are not yet mineralised, and are called "osteoid". Around the strands calcium and phosphateprecipitate on the surface of these strands, within a days to weeks becoming crystals of hydroxyapatite.[11]In order to mineralise the bone, the osteoblasts secrete vesicles containing alkaline phosphatase. This cleaves the phosphate groups and acts as the foci for calcium and phosphate deposition. The vesicles then rupture and act as a centre for crystals to grow on. More particularly, bone mineral is formed from globular and plate structures,[15][16] distributed among the collagen fibrils of bone and forming yet larger structure.[citation needed]Types
There are five types of bones in the human body: long, short, flat, irregular, and sesamoid.- Long bones are characterized by a shaft, the diaphysis, that is much longer than its width; and by an epiphysis, a rounded head at each end of the shaft. They are made up mostly ofcompact bone, with lesser amounts of marrow, located within the medullary cavity, and spongy, cancellous bone. Most bones of the limbs, including those of the fingers and toes, are long bones. The exceptions are those of the wrist, ankle andkneecap.[citation needed]
- Short bones are roughly cube-shaped, and have only a thin layer of compact bone surrounding a spongy interior. The bones of the wrist and ankle are short bones, as are thesesamoid bones.[citation needed]
- Flat bones are thin and generally curved, with two parallel layers of compact bones sandwiching a layer of spongy bone. Most of the bones of the skull are flat bones, as is the sternum.[citation needed]
- Sesamoid bones are bones embedded in tendons. Since they act to hold the tendon further away from the joint, the angle of the tendon is increased and thus the leverage of the muscle is increased. Examples of sesamoid bones are thepatella and the pisiform.[citation needed]
- Irregular bones do not fit into the above categories. They consist of thin layers of compact bone surrounding a spongy interior. As implied by the name, their shapes are irregular and complicated. Often this irregular shape is due to their many centers of ossification or because they contain bony sinuses. The bones of the spine, pelvis, and some bones of the skull are irregular bones. Examples include the ethmoid and sphenoid bones.[17]
Terminology
Main article: Anatomical terms of boneIn the study of anatomy, anatomists use a number of anatomical terms to describe the appearance, shape and function of bones. Other anatomical terms are also used to describe the location of bones. Like other anatomical terms, many of these derive from Latin and Greek. Some anatomists still use Latin to refer to bones. The term "osseous", and the prefix "osteo-", referring to things related to bone, are still used commonly today.Some examples of terms used to describe bones include the term "foramen" to describe a hole through which something passes, and a "canal" or "meatus" to describe a tunnel-like structure. A protrusion from a bone can be called a number of terms, including a "condyle", "crest", "spine", "eminence", "tubercle" or "tuberosity", depending on the protrusion's shape and location. In general, long bones are said to have a "head", "neck", and "body".When two bones join together, they are said to "articulate". If the two bones have a fibrous connection and are relatively immobile, then the joint is called a "suture".Development[edit]
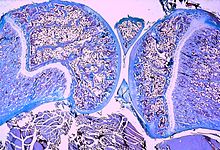
The formation of bone is called "ossification". During the fetal stage of development this occurs by two processes,Intramembranous ossification and endochondral ossification.[citation needed] Intramembranous ossification involves the creation of bone from connective tissue, whereas in the process of endochondral ossification bone is created from cartilage.Intramembranous ossification[edit]
Intramembranous ossification mainly occurs during formation of the flat bones of the skull but also the mandible, maxilla, and clavicles; the bone is formed from connective tissue such as mesenchyme tissue rather than from cartilage. The steps in intramembranous ossification are:[citation needed]- Development of ossification center
- Calcification
- Formation of trabeculae
- Development of periosteum
Endochondral ossification[edit]
Endochondral ossification, on the other hand, occurs in long bones and most of the rest of the bones in the body; it involves an initial hyaline cartilage that continues to grow. The steps in endochondral ossification are:[citation needed]- Development of cartilage model
- Growth of cartilage model
- Development of the primary ossification center
- Development of the secondary ossification center
- Formation of articular cartilage andepiphyseal plate
Endochondral ossification begins with points in the cartilage called "primary ossification centers." They mostly appear during fetal development, though a few short bones begin their primary ossification after birth. They are responsible for the formation of the diaphyses of long bones, short bones and certain parts of irregular bones. Secondary ossification occurs after birth, and forms the epiphyses of long bones and the extremities of irregular and flat bones. The diaphysis and both epiphyses of a long bone are separated by a growing zone of cartilage (the epiphyseal plate). When the child reaches skeletal maturity (18 to 25 years of age), all of the cartilage is replaced by bone, fusing the diaphysis and both epiphyses together (epiphyseal closure).[citation needed] In the upper limbs, only the diaphyses of the long bones and scapula are ossified. The epiphyses, carpal bones, coracoid process, medial border of the scapula, and acromion are still cartilaginous.[18]The following steps are followed in the conversion of cartilage to bone:- Zone of reserve cartilage. This region, farthest from the marrow cavity, consists of typical hyaline cartilage that as yet shows no sign of transforming into bone.[19]
- Zone of cell proliferation. A little closer to the marrow cavity, chondrocytes multiply and arrange themselves into longitudinal columns of flattened lacunae.[19]
- Zone of cell hypertrophy. Next, the chondrocytes cease to divide and begin to hypertrophy (enlarge), much like they do in the primary ossification center of the fetus. The walls of the matrix between lacunae become very thin.[19]
- Zone of calcification. Minerals are deposited in the matrix between the columns of lacunae and calcify the cartilage. These are not the permanent mineral deposits of bone, but only a temporary support for the cartilage that would otherwise soon be weakened by the breakdown of the enlarged lacunae.[19]
- Zone of bone deposition. Within each column, the walls between the lacunae break down and the chondrocytes die. This converts each column into a longitudinal channel, which is immediately invaded by blood vessels and marrow from the marrow cavity. Osteoblasts line up along the walls of these channels and begin depositing concentric lamellae of matrix, while osteoclasts dissolve the temporarily calcified cartilage.[19]
Function
Functions of Bone Mechanical - Protection
- Gives structure
- Facilitates movement
- Facilitates hearing
Synthetic - Contains bone marrow
Metabolic - Stores calcium
- Helps regulate the acid-base balance
Bones have a variety of functions:Mechanical
Bones serve a variety of mechanical functions. Together the bones in the body form the skeleton. They provide a frame to keep the body supported, and an attachment point for skeletal muscles, tendons, ligaments and joints, which function together to generate and transfer forces so that individual body parts or the whole body can be manipulated in three-dimensional space (The interaction between bone and muscle is studied in biomechanics).Bones protect internal organs, such as the skull protecting the brain or the ribsprotecting the heart and lungs. Because of the way that bone is formed, bone has a high compressive strength of about 170 MPa (1800 kgf/cm²),[3] poor tensile strength of 104–121 MPa, and a very lowshear stress strength (51.6 MPa).[20][21] This means that bone resists pushing(compressional) stress well, resist pulling(tensional) stress less well, but only poorly resists shear stress (such as due to torsional loads). While bone is essentially brittle, bone does have a significant degree of elasticity, contributed chiefly by collagen.Mechanically, bones also have a special role in hearing. The ossicles are three small bones in the middle ear which are involved in sound transduction.Synthetic
Cancellous bones contain bone marrow. Bone marrow produces blood cells in a process called hematopoiesis.[22] Blood cells that are created in bone marrow include red blood cells, platelets and white blood cells.[23] Progenitor cells such as thehematopoietic stem cell divide in a process called mitosis to produce precursor cells. These include precursors which eventually give rise to white blood cells, and erythroblasts which give rise to red blood cells.[24] Unlike red and white blood cells, created by mitosis, platelets are shed from very large cells called megakaryocytes.[25] This process of progressive differentiation occurs within the bone marrow. After the cells are matured, they enter the circulation.[26] Every day, over 2.5 billion red blood cells and platelets, and 50-100 billion granulocytes are produced in this way.[8]As well as creating cells, bone marrow is also one of the major sites where defective or aged red blood cells are destroyed.[8]Metabolic
- Mineral storage — bones act as reserves of minerals important for the body, most notably calcium andphosphorus.[citation needed]
- Growth factor storage — mineralized bone matrix stores important growth factors such as insulin-like growth factors, transforming growth factor, bone morphogenetic proteins and others.[citation needed]
- Fat storage — the yellow bone marrow acts as a storage reserve of fatty acids.[citation needed]
- Acid-base balance — bone buffers the blood against excessive pH changes by absorbing or releasing alkaline salts.[citation needed]
- Detoxification — bone tissues can also store heavy metals and other foreign elements, removing them from the blood and reducing their effects on other tissues. These can later be gradually released for excretion.[citation needed]
- Endocrine organ — bone controls phosphate metabolism by releasing fibroblast growth factor – 23 (FGF-23), which acts on kidneys to reduce phosphate reabsorption. Bone cells also release a hormone called osteocalcin, which contributes to the regulation of blood sugar (glucose) and fat deposition. Osteocalcin increases both the insulin secretion and sensitivity, in addition to boosting the number of insulin-producing cells and reducing stores of fat.[27]
- Calcium balance—The process of bone resorption by the osteoclasts releases stored calcium into the systemic circulation and is an important process in regulating calcium balance. As bone formation actively fixes circulating calcium in its mineral form, removing it from the bloodstream, resorption actively unfixes it thereby increasing circulating calcium levels. These processes occur in tandem at site-specific locations.[citation needed]
Remodeling
Main article: Bone remodelingBone is constantly being created and replaced in a process known as remodeling. This ongoing turnover of bone is a process of resorption followed by replacement of bone with little change in shape. This is accomplished through osteoblasts and osteoclasts. Cells are stimulated by a variety of signals, and together referred to as a remodeling unit. Approximately 10% of the skeletal mass of an adult is remodelled each year.[28] The purpose of remodeling is to regulate calcium homeostasis, repair microdamaged bones from everyday stress, and also to shape and sculpt the skeleton during growth.[citation needed]. Repeated stress, such as weight-bearing exercise or bone healing, results in the bone thickening at the points of maximum stress (Wolff's law). It has been hypothesized that this is a result of bone's piezoelectric properties, which cause bone to generate small electrical potentials under stress.[29]The action of osteoblasts and osteoclasts are controlled by a number of chemical enzymes that either promote or inhibit the activity of the bone remodeling cells, controlling the rate at which bone is made, destroyed, or changed in shape. The cells also use paracrine signalling to control the activity of each other.[citation needed] For example, the rate at which osteoclasts resorb bone is inhibited by calcitonin and osteoprotegerin. Calcitonin is produced by parafollicular cells in the thyroid gland, and can bind to receptors on osteoclasts to directly inhibit osteoclast activity. Osteoprotegerin is secreted by osteoblasts and is able to bind RANK-L, inhibiting osteoclast stimulation.[30]Osteoblasts can also be stimulated to increase bone mass through increased secretion of osteoid and by inhibiting the ability of osteoclasts to break down osseous tissue.[citation needed] Increased secretion of osteoid is stimulated by the secretion of growth hormone by the pituitary, thyroid hormone and the sex hormones (estrogens and androgens). These hormones also promote increased secretion of osteoprotegerin.[30] Osteoblasts can also be induced to secrete a number ofcytokines that promote reabsorbtion of bone by stimulating osteoclast activity and differentiation from progenitor cells.Vitamin D, parathyroid hormone and stimulation from osteocytes induce osteoblasts to increase secretion of RANK-ligandand interleukin 6, which cytokines then stimulate increased reabsorption of bone by osteoclasts. These same compounds also increase secretion of macrophage colony-stimulating factor by osteoblasts, which promotes the differentiation of progenitor cells into osteoclasts, and decrease secretion of osteoprotegerin.[citation needed]Bone volume
Bone volume is determined by the rates of bone formation and bone resorption. Recent research has suggested that certain growth factors may work to locally alter bone formation by increasing osteoblast activity. Numerous bone-derived growth factors have been isolated and classified via bone cultures. These factors include insulin-like growth factors I and II, transforming growth factor-beta, fibroblast growth factor, platelet-derived growth factor, and bone morphogenetic proteins.[31] Evidence suggests that bone cells produce growth factors for extracellular storage in the bone matrix. The release of these growth factors from the bone matrix could cause the proliferation of osteoblast precursors. Essentially, bone growth factors may act as potential determinants of local bone formation.[31] Research has suggested that trabecular bone volume in postemenopausal osteoporosis may be determined by the relationship between the total bone forming surface and the percent of surface resorption.[32]Clinical significance
See also: Bone diseaseA number of diseases can affect bone, including arthritis, fractures, infections, osteoporosis and tumours. Conditions relating to bone can be managed by a variety of doctors, including rheumatologists for joints, and orthopedic surgeons, who may conduct surgery to fix broken bones. Other doctors, such as rehabilitation specialists may be involved in recovery,radiologists in interpreting the findings on imaging, and pathologists in investigating the cause of the disease, and family doctors may play a role in preventing complications of bone disease such as osteoporosis.When a doctor sees a patient, a history and exam will be taken. Bones are then often imaged, called radiography. This might include ultrasound X-ray, CT scan, MRI scan and other imaging such as a Bone scan, which may be used to investigate cancer.[33] Other tests such as a blood test for autoimmune markers may be taken, or a synovial fluid aspirate may be taken.[33]Fractures
Main article: Bone fractureIn normal bone, fractures occur when there is significant force applied, or repetitive trauma over a long time. Fractures can also occur when a bone is weakened, such as with osteoporosis, or when there is a structural problem, such as when the bone remodels excessively (such as Paget's disease) or is the site of the growth of cancer.[34] Common fractures include wrist fractures and hip fractures, associated with osteoporosis, vertebral fractures associated with high-energy trauma and cancer, and fractures of long-bones. Not all fractures are painful.[34] When serious, depending on the fractures type and location, complications may include flail chest,compartment syndromes or fat embolism. Compound fractures involve the bone's penetration through the skin.Fractures and their underlying causes can be investigated by X-rays, CT scans andMRIs.[34] Fractures are described by their location and shape, and several classification systems exist, depending on the location of the fracture. Fractures in children are described with the Salter–Harris fracture.[citation needed] When fractures are managed, pain relief is often given, and the fractured area is often immobilised. This is to promote bone healing. In addition, surgical measures such as internal fixation may be used. Because of the immobilisation, people with fractures are often advised to undergo rehabilitation.[34]Tumours
Main article: Bone tumourThere are several types of tumour that can affect bone; examples of benign bone tumours include osteoma, osteoid osteoma, osteochondroma, osteoblastoma, enchondroma, giant cell tumor of bone, aneurysmal bone cyst, and fibrous dysplasia of bone.Cancer
Main article: Bone metastasesCancer can arise in bone tissue, and bones are also a common site for other cancers to spread (metastasise) to.[35]Cancers that arise in bone are called "primary" cancers, although such cancers are rare.[35] Metastases within bone are "secondary" cancers, with the most common being breast cancer, lung cancer, prostate cancer, thyroid cancer, and kidney cancer.[35] Secondary cancers that affect bone can either destroy bone (called a "lytic" cancer) or create bone (a "sclerotic" cancer). Cancers of the bone marrow inside the bone can also affect bone tissue, examples including leukemia and multiple myeloma. Bone may also be affected by cancers in other parts of the body. Cancers in other parts of the body may releaseparathyroid hormone or parathyroid hormone-related peptide. This increases bone reabsorption, and can lead to bone fractures.Bone tissue that is destroyed or altered as a result of cancers is distorted, weakened, and more prone to fracture. This may lead to compression of the spinal cord, destruction of the marrow resulting in bruising, bleeding and immunosuppression, and is one cause of bone pain. If the cancer is metastatic, then there might be other symptoms depending on the site of the original cancer. Some bone cancers can also be felt.Cancers of the bone are managed according to their type, their stage, prognosis, and what symptoms they cause. Many primary cancers of bone are treated with radiotherapy. Cancers of bone marrow may be treated with chemotherapy, and other forms of targeted therapy such as immunotherapy may be used.[36] Palliative care, which focuses on maximising a person's quality of life, may play a role in management, particularly if the likelihood of survival within five years is poor.Painful conditions
- Osteomyelitis is inflammation of the bone or bone marrow due to bacterial infection.
- Osteogenesis imperfecta
- Osteochondritis dissecans
- Arthritis
- Ankylosing spondylitis
- Skeletal fluorosis is a bone disease caused by an excessive accumulation offluoride in the bones. In advanced cases, skeletal fluorosis damages bones and joints and is painful.
Osteoporosis
Main article: OsteoporosisOsteoporosis is a disease of bone where there is reduced bone mineral density, increasing the likelihood of fractures.[37] Osteoporosis is defined by the World Health Organization in women as a bone mineral density 2.5 standard deviations below peak bone mass, relative to the age and sex-matched average, as measured byDual energy X-ray absorptiometry, with the term "established osteoporosis" including the presence of a fragility fracture.[38] Osteoporosis is most common in women after menopause, when it is called "postmenopausal osteoporosis", but may develop in men and premenopausal women in the presence of particular hormonal disorders and other chronic diseases or as a result of smoking and medications, specifically glucocorticoids.[37]Osteoporosis usually has no symptoms until a fracture occurs.[37] For this reason, DEXA scans are often done in people with one or more risk factors, who have developed osteoporosis and be at risk of fracture.[37]Osteoporosis treatment includes advice to stop smoking, decrease alcohol consumption, exercise regularly, and have a healthy diet. Calcium supplements may also be advised, as may Vitamin D. When medication is used, it may includebisphosphonates, Strontium ranelate, and osteoporosis may be one factor considered when commencing Hormone replacement therapy.[39]Society and culture
Bones from slaughtered animals have a number of uses. They have been used as crafting materials for buttons, handles, ornaments etc. A special genre is scrimshaw. Ground bones are used as an organic phosphorus-nitrogen fertilizer and as additive in animal feed. Bones, in particular after calcination to bone ash is used as source of calcium phosphate for the production of bone china and previously also phosphorus chemicals.[citation needed]Oracle bone script was a writing system used in Ancient china based on inscriptions in bones.To point the bone at someone is considered bad luck in some cultures, such as Australian aborigines, such as by theKurdaitcha.Osteopathic medicine is a school of medical thought originally developed based on the idea of the link between the musculoskeletal system and overall health, but now very similar to mainstream medicine. As of 2012, over 77,000 physiciansin the United States are trained in Osteopathic medicine colleges.[40]Various cultures throughout history have adopted the custom of shaping an infant's head by the practice of artificial cranial deformation. A widely practised custom in China was that of foot binding to limit the normal growth of the foot.Osteology[edit]
The study of bones and teeth is referred to as osteology. It is frequently used inanthropology, archeology and forensic science for a variety of tasks. This can include determining the nutritional, health, age or injury status of the individual the bones were taken from. Preparing fleshed bones for these types of studies can involve the process of maceration.Typically anthropologists and archeologists study bone tools made by Homo sapiensand Homo neanderthalensis. Bones can serve a number of uses such as projectile points or artistic pigments, and can also be made from external bones such asantlers.Organ (anatomy)
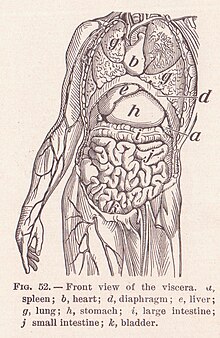
"Viscera" redirects here. For the WWE wrestler, see Viscera (wrestler).Organ  The liver of a sheep. The liver is one of the main organs in the body.
The liver of a sheep. The liver is one of the main organs in the body.Identifiers Anatomical terminology In biology, an organ (or viscus) is a collection of tissues joined in a structural unit to serve a common function.[1] In anatomy, a viscus /ˈvɪskəs/ is an internal organ, and viscera is the plural form.[2][3]Organs are composed of main tissue, parenchyma, and "sporadic" tissues,stroma. The main tissue is that which is unique for the specific organ, such as the myocardium, the main tissue of the heart, while sporadic tissues include thenerves, blood vessels, and connective tissues. Functionally related organs often cooperate to form whole organ systems. Organs exist in all higher biological organisms, in particular they are not restricted to animals, but can also be identified in plants. In single-cell organisms like bacteria, the functional analogue of an organ is called organelle.A hollow organ is a visceral organ that forms a hollow tube or pouch, such as the stomach or intestine, or that includes a cavity, like the heart or urinary bladder.[citation needed]Contents
Organ systems
Main article: Biological systemSee also: List of organs of the human bodyTwo or more organs working together in the execution of a specific body function form an organ system, also called abiological system or body system. The functions of organ systems often share significant overlap. For instance, the nervousand endocrine system both operate via a shared organ, the hypothalamus. For this reason, the two systems are combined and studied as the neuroendocrine system. The same is true for the musculoskeletal system because of the relationship between the muscular and skeletal systems.Mammals such as humans have a variety of organ systems. These specific systems are also widely studied in human anatomy.- Cardiovascular system: pumping and channeling blood to and from the body and lungs with heart, blood and blood vessels.
- Digestive system: digestion and processing food with salivary glands, esophagus, stomach, liver, gallbladder, pancreas,intestines, colon, rectum and anus.
- Endocrine system: communication within the body using hormones made by endocrine glands such as thehypothalamus, pituitary gland, pineal body or pineal gland, thyroid, parathyroids and adrenals, i.e., adrenal glands.
- Excretory system: kidneys, ureters, bladder and urethra involved in fluid balance, electrolyte balance and excretion ofurine.
- Immune System: structures involved in the transfer of lymph between tissues and the blood stream, the lymph and thenodes and vessels that transport it including the Immune system: defending against disease-causing agents withleukocytes, tonsils, adenoids, thymus and spleen.
- Integumentary system: skin, hair and nails.
- Muscular system: movement with muscles.
- Nervous system: collecting, transferring and processing information with brain, spinal cord and nerves.
- Reproductive system: the sex organs, such as ovaries, fallopian tubes, uterus, vagina, mammary glands, testes, vas deferens, seminal vesicles, prostate and penis.
- Respiratory system: the organs used for breathing, the pharynx, larynx, trachea, bronchi, lungs and diaphragm.
- Skeletal system: structural support and protection with bones, cartilage, ligaments and tendons.
Plants
Main article: Plant anatomyThe study of plant organs is referred to as plant morphology, rather than anatomy, as in animal systems. Organs of plants can be divided into vegetative and reproductive. Vegetative plant organs are roots, stems, and leaves. The reproductive organs are variable. In flowering plants, they are represented by theflower, seed and fruit. In conifers, the organ that bears the reproductive structures is called a cone. In other divisions (phylums) of plants, the reproductive organs are called strobili, in Lycopodiophyta, or simply gametophores in mosses.The vegetative organs are essential for maintaining the life of a plant. While there can be 11 organ systems in animals, there are far fewer in plants, where some perform the vital functions, such as photosynthesis, while the reproductive organs are essential in reproduction. However, if there is asexual vegetative reproduction, the vegetative organs are those that create the new generation of plants (see clonal colony).Other animals
History
Etymology
The English word "organ" derives from the Latin organum, meaning instrument, itself from the Greek word organon, implement, musical instrument, or organ of the body. The Greek word is related to ergon, work.[4] The viscera, when removed from a butchered animal, are known collectively as offal. Internal organs are also informally known as "guts" (which may also refer to the gastrointestinal tract), or more formally, "innards".Aristotle used the word frequently in his philosophy, both to describe the organs of plants or animals (e.g. the roots of a tree, the heart or liver of an animal), and to describe more abstract "parts" of an interconnected whole (e.g. his philosophical works, taken as a whole, are referred to as the "organon").The English word "organism" is a neologism coined in the 17th century, probably formed from the verb to organize. At first the word referred to an organization or social system. The meaning of a living animal or plant is first recorded in 1842.[4]Plant organs are made from tissue built up from different types of tissue. When there are three or more organs it is called an organ system.[citation needed]The adjective visceral, also splanchnic, is used for anything pertaining to the internal organs. Historically, viscera of animals were examined by Roman pagan priests like the haruspices or the augurs in order to divine the future by their shape, dimensions or other factors. This practice remains an important ritual in some remote, tribal societies.[citation needed]The term "visceral" is contrasted with the term "parietal", meaning "of or relating to the wall of a body part, organ or cavity".[citation needed] The two terms are often used in describing a membrane or piece of connective tissue, referring to the opposing sides.[citation needed]7 Vital Organs of Antiquity
Some alchemists (e.g. Paracelsus) adopted the Hermetic Qabalah assignment between the 7 vital organs and the 7Classical planets as follows:[5]Planet Organ Sun Heart Moon Brain Mercury Lungs Venus Kidneys Mars Gall bladder Jupiter Liver Saturn Spleen
Thursday, June 25, 2015
Skeletal system...
Subscribe to:
Post Comments (Atom)















ReplyDeleteIt is no secret that I have a very deep and personal relationship with God. I have pushed and resisted that relationship this past year through all the bullshit I have had to go through living with Herpes but once again, God is bigger than my stubbornness and broke through that outbreak cold sore and all I had Genital Herpes. For me personally, hearing over and over how I am not good enough has really invaded my mind in the worst way possible. I completely shut down and I was just waking up like is this how life going to end this temporary herpes outbreak “fuck everybody with herpes if you know what I mean” but let's be honest here...
It is a cowardly to say no to herbal medicine. It is fear based. And it is dishonest to what my heart wants. Don't build a wall around yourself because you are afraid of herbals made or taking a bold step especially when it's come to health issues and getting cure. So many young men/ women tell me over and over that Dr Itua is going to scam me but I give him a try to today I feel like no one will ever convince me about herbal medicine I accept Dr Itua herbal medicine because it's cure my herpes just two weeks of drinking it and i have been living for a year and months now I experience outbreak no more, You can contact him if you need his herbal medicine for any such diseases like, Herpes, Schizophrenia,Cancer,Scoliosis,Fibromyalgia,Fluoroquinolone Toxicity Syndrome Fibrodysplasia Ossificans Progressiva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic,Diabetes ,Coeliac disease,Creutzfeldt–Jakob,Dairies,Lyme Disease,Epilepsy, ,ALS,Hepatitis,Copd,Parkinson disease.Genetic disease,Fibrodysplasia disease,Fibrodysplasia Ossificans Men/Woman infertility, bowel disease ,Huntington's disease ,Diabetes,Fibroid. disease,Lupus,Lipoid Storage diseases( Gauchers disease),Polycystic Disease.,Cerebral Amyloid Angiopathy, Ataxia,Cirrhosis of Liver,Arthritis,Amyotrophic Lateral Sclerosis,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic,HIV, Epilepsy, Infertility, Love Spell,. Email..drituaherbalcenter@gmail.com then what's app.+2348149277967.... My advice to any sick men/women out there is simple... Be Always an open book. Be gut wrenching honest about yourself, your situation, and what you are all about. Don't hold anything back. Holding back will get you nowhere...maybe a one way ticket to lonelyville and that is NOT somewhere you want to be. So my final truth...and I'm just starting to grasp this one..